Helpful Tips for Patients
 Patient education is one of the most important functions of our heart failure clinics. This education comes from all members of the multidisciplinary clinic team responsible for your care and is ongoing.
Patient education is one of the most important functions of our heart failure clinics. This education comes from all members of the multidisciplinary clinic team responsible for your care and is ongoing.
This section presents some basic and easy-to-understand explanations on heart failure for you and your families. A number of handouts and check-sheets are available to help you monitor your medical condition (medications, diet, weight, exercise, hospital admissions, and emergency room visits) and keep health professionals who care for you informed of your progress.
The eight patient information sheets posted below are also supplied as information pads that are numbered for each section/topic. They are available from your clinic team:
What is heart failure?
How does a normal heart work?
 The
heart is a hollow muscle about the size of your fist. It pumps blood
with oxygen and nutrients throughout your body. The heart has four
chambers: two at the top, called atria, and two at the bottom, called
ventricles. The heart is divided into right and left sides. The right
side receives blood from the body and pumps it to the lungs to
increase its oxygen content. This blood is then pumped out to the rest
of the body by the left side of the heart.
The
heart is a hollow muscle about the size of your fist. It pumps blood
with oxygen and nutrients throughout your body. The heart has four
chambers: two at the top, called atria, and two at the bottom, called
ventricles. The heart is divided into right and left sides. The right
side receives blood from the body and pumps it to the lungs to
increase its oxygen content. This blood is then pumped out to the rest
of the body by the left side of the heart.
When you have heart failure, your heart is unable to pump enough blood to satisfy your body’s requirements. Blood that should be pumped out of the heart may back up into other organs or tissues, such as your lungs, stomach, liver, intestines or legs.
What role does the heart play in the body?
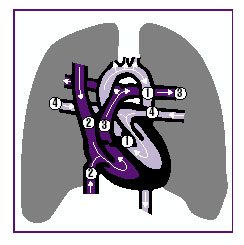 The heart is divided into left and right sides. The left side of
the heart pumps blood rich in oxygen to your muscles, skin, and organs
by means of vessels called arteries. The left side of the heart is
shown in the picture as (1). At the same time
that blood is providing nutrients and giving oxygen to the cells of
your body, it is removing waste matter from these cells. Oxygen-poor
blood, also containing waste matter, then returns to the right side of
the heart through vessels called veins (2).
The heart is divided into left and right sides. The left side of
the heart pumps blood rich in oxygen to your muscles, skin, and organs
by means of vessels called arteries. The left side of the heart is
shown in the picture as (1). At the same time
that blood is providing nutrients and giving oxygen to the cells of
your body, it is removing waste matter from these cells. Oxygen-poor
blood, also containing waste matter, then returns to the right side of
the heart through vessels called veins (2).
From there, the blood is pumped to the lungs (3) where it is
oxygenated and cleaned of carbon dioxide. It then returns to the left
side of the heart through the pulmonary veins (4) so that it may be
repumped throughout the body. Much of the waste matter accumulated
from cells is cleared by the liver and kidneys.
Why do I have heart failure?
There are many reasons why you may have heart failure. It can result from:
- A heart attack
- Your heart muscles are unable to pump effectively
- Long-term high blood pressure
- A valve in your heart may not be working properly
- You may have been drinking too much alcohol over a long period of time
- A congenital birth defect
Heart failure can be controlled. In most cases, it cannot be cured.
What are the symptoms of heart failure?
- Tiredness
- Weakness
- Cold limbs
- Loss of appetite
- Swelling in your legs and ankles
- Breathlessness
- A dry, hacking cough
- Waking up from sleep with shortness of breath or feeling smothered when you lie down to try and sleep
What treatment will I receive?
You will probably need to take several different medications, follow a low-salt diet, limit your intake of fluids, and ensure you get plenty of rest, combined with periods of exercise.
Your diet
Salt intake
![]() People
with chronic heart failure need to maintain a diet low in salt
(sodium). Sodium can make your body retain water, which may cause
swelling and stress on your heart. You may consume between 2 and 3
grams of sodium per day. It is fairly straightforward to monitor how
much salt you eat:
People
with chronic heart failure need to maintain a diet low in salt
(sodium). Sodium can make your body retain water, which may cause
swelling and stress on your heart. You may consume between 2 and 3
grams of sodium per day. It is fairly straightforward to monitor how
much salt you eat:
- Do not use the salt shaker at the dinner table. Instead of salt, use herbs, spices, garlic or salt substitutes (just make sure they do not contain potassium chloride, which could be harmful for your heart). By removing the salt shaker, you are taking an important step toward maintaining a low sodium diet.
- Do not add salt to your food during cooking.
- Check the foods you eat for salt content.
- Eat more fresh fruits and vegetables.
- Eat low-salt snacks, such as unsalted popcorn.
![]() Sodium
is found in most processed foods, including canned vegetables and
frozen dinners. Other foods and condiments high in sodium are:
Sodium
is found in most processed foods, including canned vegetables and
frozen dinners. Other foods and condiments high in sodium are:
- Cheese
- Ketchup
- Lunch meat
- Pickles
- Barbecue sauce
- Soya sauce
- Salad dressing
Learn to read food labels to determine how much salt different products contain. Ingredients in prepared food are listed in order – if salt is high on the list of ingredients, it means that there is a lot of salt in the product.
Know what counts
 |
Potassium
HF patients taking diuretics may need to increase the amount of potassium in their diet. Check with your doctor to determine if you need to increase your potassium intake. Potassium is found in:
- Chicken
- Fish
- Meat
- Bananas
- Citrus juice/fruits
- Prune juice
- Dates
- Raisins
- Mushrooms
- Potatoes
- Spinach
- Squash
- Tomatoes
Fluid intake
You need to limit the amount of fluids you drink because the more blood there is in your body, the harder your heart works. This extra work puts a strain on the heart of people with heart failure.
It is important to be aware of the amount of fluid you drink – particularly if you are taking diuretics. You should not drink too much or too little fluid. Ask your doctor or nurse to discuss with you the right amount and kinds of fluids you should be drinking. Most people with heart failure should drink no more than 6 to 8 cups of fluid per day. Remember, even the water you drink to swallow your medication should be counted. If your mouth is dry from drinking less fluid, try chewing gum. You can also take sips of water or suck on hard candies to moisten your mouth.
The following items should be considered liquids when you are calculating your daily fluid intake:
- Water
- Ice cubes
- Milk
- Coffee
- Tea
- Juice
- Soft drinks
- Bouillon
- Soup
- Wine
- Beer
- Jell-O
- Popsicles
- Ice cream
- Sherbet
- Frozen yogurt
Amount of fluid permitted daily: ____________ounces/____________mLs.
Food intake
Now that you must start paying attention to what you eat, follow Canada’s Guidelines for Healthy Eating to ensure you get the right amount of vitamins and nutrients to maintain your health.
Weight log

Exercise - take charge of your health!
![]() Physical activity is beneficial for your heart and your general health. A
regular program of physical activity will enable you to increase your strength gradually and avoid overtaxing your heart.
Physical activity is beneficial for your heart and your general health. A
regular program of physical activity will enable you to increase your strength gradually and avoid overtaxing your heart.
Exercise can:
- Help increase muscle tone and strength
- Improve your ability to function on a daily basis
- Reduce your CHF symptoms (such as shortness of breath and fatigue)
Exercise does not have to be strenuous to be valuable. (In fact, strenuous activities should be avoided.) Before you start any exercise program, be sure to:
- Discuss it with your CHF clinic physician or nurse, and set realistic goals
- Plan your exercise period when you feel the most energetic, i.e. first thing in the morning, or after an afternoon nap
- Perform activities, such as stretching, while sitting down whenever possible
- Rest frequently between periods of exercise. You may want to perform shorter activities several times per day, depending on your energy level, for example, a 10-minute walk in the morning, followed by a 10-minute stretch in the afternoon, followed by a 10-minute evening walk
Stretching exercises
Side-to-side looks: Look straight ahead, slowly turn your head to one side, hold for 10 seconds, then return to centre. Repeat 3 times on each side.
Shoulder shrugs: Sitting in a chair, slowly lift your shoulders up to your ears by squeezing your shoulder blades together, pause, then lower. Repeat 5 to 10 times.
Shoulder circles: Extend both arms sideways at shoulder height. Rotate arms 10 times in small forward circles. Repeat circling back.
Walking
Walking is a simple and effective exercise and is an ideal way to improve your activity level and get more physically fit. Here are guidelines for starting a walking program, but make sure your discuss your plans during a clinic visit before you begin.
| Week 1-2 | Walk 5 to 10 minutes |
| Week 3-4 | Walk 10 to 15 minutes |
| Week 5-6 | Walk 15 to 20 minutes |
| Week 7-8 | Walk 20 to 30 minutes |
Set personal goals
- Make exercise part of your daily routine, like brushing your teeth and showering
- Choose a friend to exercise with
- Choose a type of exercise you enjoy
- Keep a journal of your activities. This not only reinforces your exercise habits, it will also show your doctor the progress you are making.
Exercises to avoid
- Heavy lifting
- Pushing heavy objects
- Shoveling snow
- Climbing stairs
- Sit-ups or push-ups
- Competitive sports
- Heavy housework – washing windows, scrubbing floors
- Racquetball, squash, tennis
STOP exercising immediately if you:
- Become short of breath
- Feel weak, tired, or dizzy
- Feel any physical discomfort at all
- Feel your heart rate speeding up
- Have palpitations
- Are in pain
Sexual activity
Your CHF diagnosis does not mean you cannot have sex. In general, you may continue your normal sexual activities. But it is recommended that you avoid having sex:
- If you are tired or tense
- After a heavy meal
- After completing an activity that has already required you to use up a great deal of energy
Daily exercise chart
![]()
Download and print our daily exercise chart.
Medications - Your heart medication
![]() The
medication your doctor has prescribed is designed to control your
symptoms and improve the efficiency of your heart. Here are some tips
to help ensure you stick to your schedule:
The
medication your doctor has prescribed is designed to control your
symptoms and improve the efficiency of your heart. Here are some tips
to help ensure you stick to your schedule:
- Always take your medication, even if you feel well.
- Take your medications at the same times every day – make it part of your daily routine.
- Never change or stop taking your drugs before asking your doctor about it.
- Your doctor may modify the dose of your medications slightly, depending on what is best for you.
- Have all your prescriptions filled at the same pharmacy – that way, your pharmacist will get to know you and your medical history, and can counsel you appropriately.
| Medication | Action | Side effects | Recommendations |
|
Angiotensin converting enzyme (ACE) inhibitors
Also called: |
• Widens (dilate) blood vessels. |
• Weakness. |
• Take this medication at the same time
each day. |
|
Angiotensin II receptor antagonists*
Also called: |
• Widens (dilate) blood vessels. |
• Weakness. |
• Take this medication at the same time
each day. |
|
Beta-blockers
Also called: |
• Slows heart rate. |
• Weakness, tiredness. |
• Take this medication at the same time
every day. |
|
Diuretics
Also called: |
• Eliminates water and salt (sodium) from
your body. |
• Frequent urination. |
• Take this medication with meals to avoid
stomach upset. |
|
Digitalis/digoxin
Also called: |
• Increases the strength and efficiency of
your heart’s pumping action. |
• Nausea. |
• Take this medication on an empty stomach. • Never change brands or take extra pills. |
|
Nitrates/nitroglycerin & vasodilators*
Also called: |
• Expands your blood vessels, making your heart pump more easily. |
• Fluid retention. |
• Take this medication with liquid at mealtimes. |
|
Anticoagulants & antiplatelets*
Also called: |
• Thins your blood to prevent clots from forming. |
• Hemorrhaging (bleeding), which may result in feelings such as headache, chest, abdomen or joint pain, dizziness, shortness of breath, difficulty breathing or swallowing, swelling, or weakness. |
• Take your dose as soon as possible on the same day if you’ve forgotten, but don’t take a double dose the next day to make up for missed doses. |
|
Inotropic agents
Also called:* |
• Helps your heart pump more effectively. |
• Nausea, vomiting. |
• Inotropic agents are administered intravenously while you are in hospital. |
|
Calcium channel blockers*†
Also called: |
• Used to treat the high blood pressure often associated with heart failure. |
• headaches, facial flushing and dizziness, ankle swelling. |
• These medications are not used often to
treat heart failure. |
|
Potassium*† |
• Since most diuretics remove potassium from the body, heart failure patients who use them are at risk of losing too much potassium. Some patients need to take potassium supplements or pills to compensate for the amount they're losing. |
• ACE inhibitors can actually cause the body to retain potassium, so this needs to be taken into account as well. Patients should check with their doctors to determine their potassium needs. |
• Instead of potassium, sometimes all is
needed to do is eat foods high in potassium, such as bananas. |
*Draft changes pending adoption by CHFN
†Adopted from
Medications Commonly Used to Treat Heart Failure, American Heart
Association
Medical/Medication history
![]() Please use this sheet to record important changes in your medical condition
that you should report during your CHF clinic visits. This information
will help your doctors and nurses to better manage your care.
Please use this sheet to record important changes in your medical condition
that you should report during your CHF clinic visits. This information
will help your doctors and nurses to better manage your care.
Follow-up care
![]() If your heart failure has been determined to be stable, you should be
visiting the heart failure clinic every three to six months, or you
may be asked to see your family doctor. Your doctor or nurse will tell
you how often you should visit the clinic. During these visits certain
procedures will be done, including:
If your heart failure has been determined to be stable, you should be
visiting the heart failure clinic every three to six months, or you
may be asked to see your family doctor. Your doctor or nurse will tell
you how often you should visit the clinic. During these visits certain
procedures will be done, including:
- Doing blood tests
- Checking your medications
- Reviewing your diet
- Discussing your exercise routines
If your heart failure has been determined to be unstable, you should be visiting the heart failure clinic daily or weekly. Your doctor or nurse will tell you how often is appropriate. During these visits certain procedures will be done, including:
- Assessing your physical state
- Discussing how well you’re following your medication schedule
- Adjusting your medications, if necessary
- Doing lab tests, if required
- Reviewing your diet
- Discussing what exercise/activity you can do
The clinic’s main aim in seeing you frequently during this time is to ensure you don’t have to be admitted to hospital, and to help you function better at home.
Your clinic's 'telemanagement' program
Telemanagement means that should you need to call your clinic with any questions or concerns, feel free to do so at any time. A clinic nurse will be available to assist you.
Your clinic’s telephone support hotline number is: ____________________
Should you need to call after hours, the pager number is: ________________
Your clinic support group
Your HF clinic has started a support group to help you meet other patients and to learn more about your disease from health care experts.
The next support group meeting will be held: _______________________
The speaker will be: ______________________________________
She/he will be speaking about: ________________________________
We look forward to seeing you there!
Tips for coping
![]() Controlling the anxiety you may be feeling after being diagnosed with CHF is very
important to your overall well-being. There are many ways to control
anxiety. Here are some suggestions:
Controlling the anxiety you may be feeling after being diagnosed with CHF is very
important to your overall well-being. There are many ways to control
anxiety. Here are some suggestions:
- Write a list of your worries or causes of anxiety. Sometimes just putting pen to paper will help ease your concerns and put things in perspective.
- Try to think of solutions in keeping with the requirements and
restrictions of your illness. For example:
- Surround yourself with positive people
- Learn relaxation techniques – such as deep breathing or meditation
- Talk about your frustrations with those you love and trust
- Consult a resource person – your clinic nurse, social worker or counsellor
- Know and accept your limitations: learn to say no without feeling guilty
- Indulge yourself without feeling guilty. Fulfil a desire in keeping with your lifestyle and pocketbook – for example, go to the theatre, take a holiday, buy an item of clothing or object you’ve been craving
Resources – Booklets
![]() Managing Congestive Heart Failure* (free)
Managing Congestive Heart Failure* (free)
Published by: The Heart and Stroke Foundation of Canada
Heart and Stroke Foundation of Canada
Ontario Chapter
477 Mount Pleasant Road, 4th Floor
Toronto, Ontario M4S 2L9
Living with congestive heart failure: (free)
a guide for people taking Coreg™*
Edited by Peter Liu, MD and Shanas Mohamed, RN
Published by: SmithKline Beecham Pharma
Phone: 1 800 567-1550
SmithKline Beecham Pharma
Medical Information Department
2030 Bristol Circle Place
Oakville, Ontario L6H 5V2
A stronger pump: A guide for people with heart failure (cost:
U.S. $6.50 per copy)
Published by: Pritchett & Hull Associates
Phone: 1 800 241-4925
Pritchett & Hull Associates
3440 Oakcliffe Road, Suite 110
Atlanta, Georgia 30340-3079
Dietary fats and your heart: action plan for a healthy heart*
(free)
Published by: The Becel Heart Health Information Bureau
Phone: 1 800 563-5574
Becel Heart Information Bureau
160 Bloor Street, Suite 1500
Toronto, Ontario M4W 3R2
An owner’s manual for patients with congestive heart failure
(cost: $2.00 per copy)
Contact: Rosa Gutierrez, RN MScN
Walter McKenzie Centre
2C2 Cardiology
8440 – 112 Street
Edmonton, Alberta T6G 2B7
Phone: 403 492-8157
Fax: 403 492-6452
* available in English and French