Clinic Resource Manual
 This resource manual has been developed by the CHFN to assist its members in the operation of a heart failure (HF) outpatient clinic. It provides an overview of a management structure for the clinic, identifies the clinic team, and describes the roles and responsibilities of each team member. The manual will be updated periodically by the education subcommittee.
This resource manual has been developed by the CHFN to assist its members in the operation of a heart failure (HF) outpatient clinic. It provides an overview of a management structure for the clinic, identifies the clinic team, and describes the roles and responsibilities of each team member. The manual will be updated periodically by the education subcommittee.
The current edition (Second Edition, August 2010) of the resource manual is divided into seven (7) parts. These parts correspond to the seven (7) sections of the resource manual listed below:
Preface
Heart failure (HF) has been a growing clinical problem in Canada and throughout the world resulting in reduced quality of life, recurrent hospitalizations and premature death.
Mission Statement
The mission of the Canadian Heart Failure Network (CHFN) is to provide appropriate, comprehensive, high-quality care to limit disability and improve the quality of life of patients with HF through exemplary outpatient management in outpatient HF clinics. Each clinic will be a centre of excellence for the clinical management of HF and will also serve as a resource centre dedicated to improve the quality and quantity of life for HF patients and their families.
About this Manual
This resource manual has been developed to assist health care professionals in the successful operation of a HF outpatient clinic. It provides an overview of a management structure for the clinic, identifies the clinic team, and describes the roles and responsibilities of each team member. A multidisciplinary approach is recommended where Physicians, Nurses, Dieticians, Pharmacists and other health care professionals provide collaborative advice and direction.
Because patient compliance is a key factor in the management of HF, an extensive patient education program is also included in this manual.
Medical management, care protocols and patient monitoring are key elements of the HF clinic and are included as guidelines to assist in the optimization of HF care across Canada.
Data collection using a flexible data-gathering tool is used to guide current and future practice, measure outcomes, determine quality of life (QOL) issues and track patient satisfaction. Periodic analyses of data collected allows practitioners to review and change practice patterns to enhance patient care and QOL. Ongoing data collection will also allow practitioners to demonstrate the cost-benefits derived from treating HF in the clinic setting.
This resource manual will be updated periodically as warranted by new research findings, changes in clinical practice guidelines, and continuing clinical experience.
Disclosure
This website was developed by the Canadian Heart Failure Network (CHFN) as an aid for health care professionals, heart failure patients, and lay persons to better understand heart failure and how it may be prevented and treated. The information and opinions provided are not a substitute for normal medical care provided by Physicians or other health care professionals, and are for general interest only. The advice and information do not constitute recommendation for changes in treatment for any particular individual, and the information may not apply to all patients or clinical situations. Mention of specific products, processes or services does not constitute or imply a recommendation or endorsement by the CHFN.
The CHFN assumes no liability arising from any error or omission in the information available on the website and recommends that you confirm with your Physician if a change in your management is required. Links to other websites are for your information and convenience only and CHFN accepts no responsibility or liability for the content or any advice in those external websites. When you link to an external website, you have left the CHFN website and the CHFN is not responsible for the privacy policies or content located within these external sites.
Sponsorship
This program is an independent national network with initial support from SmithKline Beecham Pharma and Hoffmann-La Roche and ongoing support from our corporate partners.
The impetus for the program came from Cardiology Physicians and Nurses from across Canada who envisioned the need for a common and comprehensive approach to the current management of patients with HF.
Comments/Suggestions
We welcome any comments and suggestions you may have regarding this important educational program. Kindly send them to:
Malcolm Arnold, MD, FRCPC, FACC
Chair, Working Group
Canadian Heart Failure Network (CHFN)
University Hospital - London Health Sciences Centre
C6-124D
339 Windermere Road
London, Ontario
N6A 5A5
www.chfn.ca
T: 519-663-3496
F: 519-663-3497
Rationale for HF Clinics
The Problem: Heart Failure
Heart failure (HF) is a major health problem in Canada and throughout the world. Presently, HF affects 5 million to 7 million North Americans and another 20 million individuals in Third World countries.1
In Canada, HF affects more than 1% of the population and is responsible for 9% of all deaths. HF is the most common cause of hospitalization of people over 65 years of age.2
The incidence and prevalence of HF will continue to rise as the population ages. As shown in Figure 1.1, it is estimated that HF prevalence will nearly double due to the aging population by the year 2030.3 In some regions of Canada, the rate of HF is increasing by as much as 4% annually.
Despite medical management, recent data suggest that the HF mortality rate may be as high as 40% to 50% two years following treatment.4 In addition, the continual cycles of acute crises associated with HF result in high hospital readmission rates and increased health care costs.
This steady increase in the number of deaths, hospitalizations, and medical costs associated with HF continues to occur at a time when morbidity and mortality rates from other common cardiovascular diseases (such as myocardial infarction) are on the decline.
There is an urgent need for aggressive measures to reduce the mortality and morbidity associated with HF, reduce hospital admissions and readmissions, and improve patient management.

|
One Solution: HF Clinics
In recent years, a number of HF clinics have been established in Canada and the United States in an effort to improve the quality of life of patients with HF and reduce the economic burden associated with the inpatient management of this patient population.
Preliminary findings from the Cardiology Preeminence Roundtable publication suggest that progress in the management of patients with HF depends on avoiding hospitalization in the first place.3
Figure 1.2 shows several approaches that are being successfully used to manage HF patients in the outpatient setting. 3
“As much as 50% of inpatient care for HF ideally should have occurred elsewhere or been avoided altogether.”
Cardiology Preeminence Roundtable3

|
As shown in Figure 1.3, heart failure
clinics have the potential to reduce length of stay
and hospital admissions.3
“Outpatient intervention not only reduces HF admissions, but when hospitalization is unavoidable, it reduces the average length of stay.”
Cardiology Preeminence Roundtable3

|
Heart Failure
Heart failure (HF) is a state in which the heart is unable to pump blood at a rate to meet the requirements of metabolizing tissues or can only do so from an elevated filling pressure. Many forms of heart disease may lead to heart failure. Other diseases and treatments can precipitate exacerbations of HF.
Etiology of Heart Failure
- Ischemia/myocardial infarction 65%
- Non-ischemic dilated cardiomyopathy 20%
- Other 15%
Ischemia and/or myocardial infarction contribute to the development of heart failure in up to 65% of cases.5 Myocardial infarction can lead to ventricular remodelling with compensatory dilation and hypertrophy and subsequent systolic and diastolic dysfunction progressing to the clinical syndrome called HF. In patients with ischemia, the major cause of heart failure is systolic dysfunction with some degree of diastolic dysfunction.
In a subgroup of patients, the cause of heart failure is diastolic dysfunction. These individuals have signs and symptoms of heart failure but a normal left ventricular ejection fraction. Appropriate management of these patients is to address the underlying etiology. Unfortunately, there are few clinical trials to direct decisions about the best choice of drug therapy.
Some patients have signs of HF such as cardiomegaly on chest x-ray or left ventricular dysfunction, but no symptoms.
Goals of Heart Failure Treatment
The clinical goals of heart failure treatment are to:
- Improve heart function
- Reduce symptoms
- Prevent hospital readmissions
- Improve survival
- Improve quality of life
Disease Progression in Heart Failure
Most patients with heart failure have only mild symptoms and often respond well to medical therapy. Unfortunately, because of the progressive nature of HF, these patients remain at risk for worsening disease despite the optimal use of current firstline medications. This is because myocardial damage triggers a series of compensatory mechanisms that progressively compromise cardiac function.
In the early stages of myocardial damage, activation of neurohormonal systems, including the renin-angiotensin-aldosterone (RAA) and sympathetic nervous systems, provides initial support for the failing heart. However, the continued neurohormonal activation becomes deleterious with excessive vasoconstriction, volume expansion, and ventricular remodelling leading to continued deterioration in cardiac function.
Ventricular remodelling can be favourably altered by angiotensin-converting enzyme (ACE) inhibitors, agents that have been shown to reduce morbidity and mortality in patients with HF and asymptomatic left ventricular dysfunction.6
Recent clinical findings suggest that beta-blockers can reduce symptoms, improve left ventricular function, and inhibit disease progression in patients with mild to moderate HF on standard therapy consisting of an ACE inhibitor and diuretics, with or without digoxin.7-10
Emerging data on the beneficial effects on outcome in heart failure patients with beta1-selective blockers further support the importance of this therapy.11,12 However, in a meta-analysis of the clinical effects of beta-adrenergic blockade in heart failure, Lechat and colleagues reported that the reduction in mortality risk was greater for nonselective beta-blockers than for beta1–selective agents.10
Diuretics are very successful in reducing symptoms of HF and they probably reduce readmissions for heart failure. However, their influence on survival has not been adequately tested. Digoxin can improve symptoms and will reduce hospital readmissions for heart failure, but has a neutral effect on survival. Some positive inotropic agents will reduce symptoms and hospital readmissions for heart failure, but may worsen the underlying disease process.
References
- Ackman ML, Harjee KS, Mansell G, et al. Cause-specific noncardiac mortality in patients with chronic heart failure — a contemporary Canadian audit. Can J Cardiol 1996;12:809-813.
- Brophy JM. Epidemiology of chronic heart failure. Canadian data from 1970-1989. Can J Cardiol 1992;8:495-498.
- Cardiology Preeminence Roundtable. Beyond Four Walls: Cost-Effective Management of Chronic Congestive Heart Failure. Washington, D.C.: Advisory Board Company, 1994.
- Johnstone DE, Abdulla A, Arnold JMO, Bernstein V, et al. Diagnosis and management of heart failure. Can J Cardiol 1994;10:613-631.
- Canadian Cardiovascular Society. Report on the 1993 Consensus Conference on the Diagnosis and Treatment of Heart Failure. Toronto: Queen’s Printer for Ontario, 1996.
- The SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992;327:685-691.
- Doughty RN, Whalley GA, Gamble G, MacMahon S, Sharpe N. Left ventricular remodeling with carvedilol in patients with chronic heart disease due to ischemic heart disease. J Am Coll Cardiol 1997;29:1060-1066.
- Packer M, Bristow MR, Cohn JN, et al, for the U.S. Carvedilol Heart Failure Study Group. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349-1355.
- Heidenreich PA, Lee TT, Massie BM. Effect of beta-blockade on mortality in patients with heart failure: a meta-analysis of randomized clinical trials. J Am Coll Cardiol 1997;30:27-34
- Lechat P, Packer M, Chalon S, Cucherat M, Arab T, Boissel J-P. Clinical effects of ß-adrenergic blockade in chronic heart failure. Circulation 1998;98:1184-1191.
- CIBIS Investigators and Committees. A randomized trial of ß-blockade in heart failure: the Cardiac Insufficiency Bisoprolol Study (CIBIS). Circulation 1994;90:1765-1773.
- The International Steering Committee on Behalf of the MERIT-HF Study Group. Metoprolol CR/XL. Randomized Intervention Trial in Heart Failure (MERIT-HF): rationale, design, and organization. Am J Cardiol 1997;80(Suppl 9B):54J-58J.
*Draft changes pending adoption by CHFN
The HF Clinic
Establishing a Heart Failure Clinic
Informing the Community
HF clinics offer an effective alternative to the current cycle of acute care management. They offer complete patient evaluations, education, regular monitoring, and immediate response to patients’ clinical needs.
In addition, HF clinics offer long-term benefits to patients, families, and the communities they serve. It is expected that each local HF clinic will be a centre of excellence for the clinical management of HF and a resource centre dedicated to improving the lifestyle of HF patients and their families.
Objectives of Heart Failure Clinics
- Improve patient care
- Provide medical care in a timely fashion
- Optimize the use of proven medical therapies
- Educate HF patients about all aspects of their condition
- Improve cardiac function
- Improve quality of life
- Empower patients with the knowledge/capacity to manage heart failure
- Reduce hospital admissions and readmissions
- Reduce morbidity and mortality
- Disseminate the latest information on HF
- Serve the community
- Quality of care assessment
Facility Profile
Clinic Accommodations
- Examination rooms, waiting area, meeting room, offices, exercise room, telemonitoring, telephone follow-up
Equipment
- Office equipment, computers, tables, chairs, blood pressure machines, scales, echocardiograph, treadmill, bikes
Operating Costs
- Part-time cardiologist(s)
- Full-time clinic staff: nurse manager/coordinator, clerical staff
- Telephone costs, Internet access
- Clinic supplies, office supplies

Access/Referral to
- Electrophysiology, CRT, ICD
- Cardiac Surgery
- Transplantation team
HF Clinic Team
The clinics will be Physician-directed and Nurse-managed. The on-staff Cardiologist will perform all initial assessments and examinations, and then develop a treatment plan that will be implemented and managed by the Clinic Nurses.
The Nurse Manager/Clinic Nurse is experienced in cardiology and may have some experience in the outpatient setting. In many settings, Nurses with advanced training are responsible for patient management and the implementation of delegated medical tasks.
Along with the Nurse(s) and the Cardiologist, the clerical staff are considered primary members of the clinic team. They will perform daily administrative duties and assist in data collection and data entry.
Secondary team members who may be affiliated with the clinic on either a part-time, full-time, or referral-only basis include: Pharmacists, Dietitians, Psychologists, Social Workers, and Exercise Physiologists or Physical Therapists as well as EEP Cardiologists and Cardiac Surgeons.
Pharmacists are important members of the clinic’s multidisciplinary team. They provide both patients and staff with information concerning drug interactions, pharmacokinetics of drug action, side-effects of medications, and dosing adjustments required for comorbid conditions. Counselling by a Clinical Pharmacist has been shown to increase patient compliance with medication regimens, resulting in improvements in peripheral edema and physical capacity.1,6
Referrals to a Registered Dietitian are particularly important for HF patients suffering from comorbid conditions such as diabetes or renal failure. The Dietitian will educate patients about the need for sodium and fluid restriction, assess protein and caloric requirements, and incorporate dietary changes needed to manage comorbid conditions.
Depression, anger, and frustration related to decreased quality of life are common among HF patients, particularly those patients with poor psychosocial adjustment to their situation.2 Therefore, referral to a Clinical Psychologist may be necessary. Counselling by a Psychologist can help patients and their family members adjust emotionally to the difficult lifestyle changes required for HF management.
The primary role of the social worker is to develop an individualized living plan for the HF patient. This plan may include making arrangements for food/meals, transportation, home assistance, and providing access to financial assistance. The Social Worker can also assist patients and their family members in finding support groups that provide open discussions of common issues such as work, sexuality, exercise and leisure activities, and the adjustments that must be made to each.
Although HF patients have traditionally been encouraged to modify physical activity, exercise rehabilitation programs have been used successfully to improve the functional capacity of HF patients.3,4 Therefore, an Exercise Physiologist or Physical Therapist may be affiliated with the clinic to establish an appropriate exercise regimen for the HF patient, provide instruction on exercise limitations, and monitor the exercise program.
In addition to the secondary team members, heart failure clinics may be affiliated with Occupational Therapists, Home-care Providers, Palliative-care Physicians, patient-support groups, transplant teams, members of the clergy, and volunteers. Although not core members of the clinic team, these individuals are highly valued members of a successful clinic program. For example, Home-care Providers are particularly important for the management of older HF patients who may have difficulty performing daily activities such as bathing and sitting in a chair. Also, palliative-care counselling may be required for the emotional well-being of both patients and their family members. Many patients find psychological relief in the ability to talk openly about the mortality associated with heart failure, and preparation for death.5,6,7,8,9
Patient Selection
Heart failure clinics are outpatient facilities that offer a comprehensive approach to HF management. All patients with suspected and established heart failure (NYHA Classes I to IV) should be eligible for treatment at these clinics. Referrals to the HF clinic are accepted from any source: community Physicians, hospital-based Physicians, and other clinics. Nurse and patient-facilitated referrals for education may also be accepted.
| Clinic director | Responsibilities |
| Cardiologist | • Receives patient referrals • Performs initial evaluations • Establishes medical regimen • Sees patient regularly • Liaises with Nurse Manager before any major changes in medical intervention |
| Nurse Manager
Registered Nurse with cardiology experience |
• Implements treatment plan • Educates patient • Adjusts medications (using drug management protocols) • Schedules patient appointments • Makes regular follow-up calls |
As shown in Figure 2.1, patient education
is key to the success of a HF management
program. Education should involve all members of the multidisciplinary
clinic team and
should be ongoing.
Data Collection
Data collection can be used by heart failure clinics for the following purposes:
- To monitor patient care issues and outcomes
- To track public health data
- To document the need for the clinic
- To secure funding
- To answer research questions
References
- Uretsky BF, Pina I, Quigg RJ, Brill JV, et al. Beyond drug therapy: nonpharmacologic care of the patient with advanced heart failure. Am Heart J 1998;135(Suppl 2):S264-S284.
- Dracup K, Walden JA, Stevenson LW, Brecht M-L. Quality of life in patients with advanced heart failure. J Heart Lung Transplant 1992;11:273-279.
- Coats AJS, Adamopoulos S, Radaelli A, et al. Controlled trial of physical training in chronic heart failure. Circulation 1992;85:2119-2131.
- Sullivan MJ, Higginbotham MB, Cobb FR. Exercise training in patients with severe left ventricular dysfunction. Circulation 1998;78:506-515.
- Hauptman PJ, Rich MW, Heidenreich PA et al. The Heart Failure Clinic: A consensus statement of the Heart Failure Society of America. J. Card Failure 2008; 14: 801-815.
- Gattis WA, Hasselblad V. Whellan DJ, O'Connor CM. Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team: Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study. Arch. of Internal Medicine 1999;159(16): 1939-1945.
- Albert NM, Fonarow GC, Yancy CW et al. Influence of dedicated heart failure clinics on delivery of recommended therapies in outpatient cardiology practices: Findings from the Registry to improve the use of Evidence - Based heart Failure Therapies in the Outpatient Setting (Improve HF). Am Heart J 2010; 159:238-44.
- McAlister FA, Stewart S, Ferrura S, McMurray JJJV. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: A systematic review of randomized trials. J. Am Coll. Cardiol.2004; 44:810-819.
- Focused Update Incoporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: A Report of the American College of Cardiology Foundation / American Heart Association Task Force on Practice Guidelines. Circulation 2009;119:391-479.
*Images provided by Microsoft Clip Art
Medical Management
Running a Heart Failure Clinic
1. Scope
This document provides strategies for the improved diagnosis and management of adults (19 years and older) with heart failure (HF). It is intended for primary care practitioners, allied health professionals and patients with HF. It focuses on approaches needed to provide care to patients with this complex syndrome.
2. Diagnostic Code:
428
3. Clinical Highlights
HF is a complex syndrome associated with a high rate of hospitalization and short-term mortality, especially in elderly patients with comorbidities. Early diagnosis and treatment can prevent complications.
- Successful HF management begins with an accurate diagnosis. All patients should have an objective determination of left ventricular ejection fraction (LVEF) by echocardiogram, or radionuclide ventriculogram (RNV) if echocardiogram is unavailable
- Treat underlying vascular risk factors (see guidelines on Hypertension and Diabetes Care), comorbidities and other chronic diseases
- Patient and caregiver education should be tailored and repeated
- Encourage the patient to accept responsibility for their HF care through an individualized management plan with self-care objectives, including salt restriction, weight monitoring and medication adherence strategies
- Reinforce the importance of healthy lifestyle modifications, including healthy eating, regular exercise, weight management, social support and smoking cessation
- Treatment requires combination drug therapy
- All systolic HF patients should receive an ACE-I and a BB at target dose unless contraindicated. These therapies should be considered in all patients with HF with preserved systolic function (PSF)
- Additional therapy should be guided by clinical situation
- As polypharmacy remains a concern - match drugs to goals of treatment
- Care should be individualized based on symptoms, underlying cause, disease severity and goals of care
- Plan effective systems to ensure follow-up and patient education to improve outcomes
- Engage patients in open discussions on the end of life issues
4. Prevention of Heart Failure
- Assess all patients for known or potential risk factors for HF (hypertension, ischemic heart disease, diabetes mellitus, dyslipidemia and tobacco use)
- Modifiable risk factors should be treated according to current guidelines
- Routine screening for asymptomatic LV dysfunction is currently not recommended
- For selected patients at high risk for HF due to multiple risk factors, the decision to screen (such as by echocardiography) should be individualized
- The prognosis of HF at the earliest appropriate time
5. Patients with Asymptomatic LV Dysfunction
- ACE-I should be used in all asymptomatic patients with LV dysfunction and
LVEF < 40% - BB should be considered in all patients with asymptomatic LV dysfunction
and LVEF < 40% (especially if there is a history of ischemic heart disease)
6. Diagnosis of Heart Failure
HF is under diagnosed in its early stages. Diagnostic accuracy improves when there is a high index of suspicion and a consistent approach to diagnosis.
7. Definition of Heart Failure
HF is a clinical syndrome defined by symptoms suggestive of impaired cardiac output and/or volume overload with concurrent cardiac dysfunction. While a normal LVEF is >60%, the threshold of 40% is used for the purposes of diagnostic classification. As such, HF can be classified into systolic heart failure, as defined by the presence of signs and symptoms of HF with an LVEF <40%, and heart failure with preserved systolic function (HF with PSF – previously called diastolic dysfunction) is defined by the presence of signs and symptoms of HF in the absence of systolic dysfunction (LVEF ≥ 40%). Prognosis for systolic HF is significantly worse than HF with PSF. Research evidence for treatment is best established for systolic HF but, in general, the pharmacologic and nonpharmacologic strategies are similar for both.
8. Evaluation of HF should include:
- A thorough history and physical exam focusing on:
- Current and past symptoms of HF (i.e. fatigue, shortness of breath, diminished exercise capacity and fluid retention/weight gain)
- Functional limitation by New York Heart Association (NYHA)
- Cardiovascular risk factors, cardiovascular disease, and other comorbid conditions
- Assessment of a patient’s endurance, cognition, and ability to perform activities of self-management and daily living
- Assessment of volume status (e.g. peripheral edema, rales, hepatomegaly, ascites, weight, jugular venous pressure, and postural hypotension)
- Initial investigations in all patients (where available):
- Complete blood count
- Serum electrolytes
- Creatinine (Cr), eGFR
- Urinalysis
- Microalbuminuria
- Fasting blood glucose
- Fasting lipid profile, AST
- Albumin
- Thyroid-stimulating hormone (TSH)
- 12-lead electrocardiogram and chest radiograph
- All patients should have an objective determination of LVEF by transthoracic echocardiogram (preferred as it also provides information on cardiac dimensions, valvular function and may suggest the underlying etiology of HF) or RNV if echocardiogram is unavailable
- BNP has high diagnostic value for both types of HF and is recommended where available, when diagnosis is unclear. The use of BNP in non-acute heart failure and community outpatient practice remains to be clarified. (See Table 1)


- In cases where there is doubt, or an objective determination of LVEF is not immediately available, response to a therapeutic trial may increase the diagnostic accuracy (See Figure 1)
- When the etiology of HF is uncertain, consider referral for more specialized cardiac testing as clinically indicated

9. Non-Pharmacologic Management Strategies
HF care depends on the patient’s understanding of, and participation in, optimal care. Patients can be important partners in individualized goal setting, salt restriction, weight monitoring, and adherence.
9.1. Goals of Care
- Determine the goals of managing their HF with the patient, i.e. aggressiveness from a goal of an advanced cardiac technology and transplantation through to a goal of symptom control and palliation
- Identify an appropriate substitute decision maker (health proxy)
- Advance Directives / Representation Agreements regarding end-of-life care should be addressed at the earliest appropriate time
- Above decisions should be reviewed regularly and specifically when there is a change in the patient’s clinical status
9.2. Self-Monitoring
- Discuss the importance of self-management with the patient and their network of support
- Work with the patient on the specifics of the plan as outlined below (9.3-9.9)
9.3. Weight
- All patients should be encouraged to weigh themselves daily and recognize symptoms of worsening HF
- Initially: Report a weight gain of 2.5 kg/week or a worsening of symptoms
- Goal: Self-assessment and adjustment of fluid/sodium restriction and/or diuretic dosing in response to a weight gain of ≥1 kg (patient-based algorithm)
9.4. Salt Intake
- All HF patients should limit sodium intake, avoid processed foods and avoid adding salt
- Review salt intake when weight gain is experienced

9.5. Fluid Intake
All HF patients with hyponatremia, or severe fluid retention/congestion that is not easily controlled with diuretics, should limit fluid intake to 6-8 cups of liquid/day (1 cup = 8 ounces = 250 mL), including frozen items and fruit (1 serving = 1/2 cup of liquid).
9.6. Alcohol
Not more than one drink per day is recommended. This is equal to a glass of wine (5 oz./150 mL/12% alcohol), beer (12 oz./350 mL/5% alcohol), or one mixed drink (1 1/2 oz./50 mL/40% alcohol). In alcohol related heart failure, alcohol must be totally avoided.
9.7. Exercise Training
- All HF patients with stable symptoms and volume status should undertake regular, moderate intensity physical activity (aerobic and resistance exercises to maintain muscle mass)
- Aerobic physical activity: Start with 5-10 minute sessions every other day, working to a goal of 30-45 minutes per day 4-5 days per week
- Resistance exercises (do 10-15 repetitions at 50-60% of normal effort)
9.8. Immunization
All HF patients should be immunized for influenza (annually) and pneumococcal pneumonia (if not received in the last six years) to reduce the risk of respiratory infections.
9.9. Collaboration with complementary health care providers
- Involve Nurses, Pharmacists, Dieticians and Cardiac Exercise Therapists for individual or group visits when possible
- A Dietician can provide valuable education regarding the practical aspects of implementing a salt and water restriction, how to make healthy food choices and/or a group grocery store tour to help facilitate low-salt food and drink selections
- A Pharmacist may help patients remain on therapy when they are faced with side-effects and provide useful advice to help with medication compliance
- A Cardiac Exercise Therapist may be instrumental in helping HF patients develop and continue a structured exercise program
10. Pharmacotherapy for Heart Failure
- In general, research evidence for treatment is best established for systolic HF, although the underlying principles and pharmacotherapy also apply to HF with PSF. However, when treating HF with PSF, extra caution is required with ACE-I, vasodilators and diuretics to prevent symptomatic hypotension or pre-renal failure as LV filling pressures are volume dependent
- It is important to treat the following underlying cause where possible, especially in the case of HF with PSF:
- Hypertension (goal is blood pressure <140/90 mmHg)
- Ischemic heart disease
- Atrial fibrillation (goal ventricular rate between 60-80 at rest and <110 with exercise)
- Hypertrophic cardiomyopathy (consider referral to specialist)
- All patients with systolic HF should be on an ACE-I and a BB unless contraindicated (these medications should be strongly considered in patients with HF with PSF)
- Historically, an ACE-I was started first and titrated to target dose before starting a BB but current evidence suggests that it does not matter which drug is started first as long as both are titrated to target dose
- See Appendices regarding medication initiation and titration - BB should not be initiated in patients with volume overload
- ARB can be substituted for BB or ACE-I if they are not tolerated
- ARB can be cautiously added to patients with persistent symptoms despite optimal ACE-I and BB dose
- In the elderly, initial doses should be low and titrated slowly
- Concerns may arise as these medications are titrated upwards
Blood Pressure:
- When the systolic BP is below 80 mmHg, limit increase in medication if the patient shows symptoms of low BP (consider measuring postural vitals in the elderly)
- Take blood pressure lowering medication with food
- Separate the dosing of blood pressure lowering medications by at least 2 hours (i.e. give the ACE-I at noon and BB in the morning and at bedtime)
- If hypotension occurs during medication titration consider:
- Adding a higher dose at bedtime first, then increase the morning dose (if BID dosing)
- Decrease or discontinue the diuretic and/or vasodilator
- Consider temporarily reducing the ACE-I dose during BB titration
- Decrease the BB dose by 50% and reinitiate titration once condition stabilizes
Renal Function:
- If Creatinine (Cr) increases by >30% evaluate the patient’s volume status and consider reducing/holding diuretic (if volume deplete) before reducing/holding digoxin, ACE-I, ARB, spironolactone or BB
- Referral to a Nephrologist is encouraged when there is kidney impairment as defined by a Cr increase by >30%, an eGFR <30 mL/min or eGFR <45 mL/min if cause is unknown
- If a drug with proven mortality benefit is not tolerated by the patient (because of hypotension, bradycardia or progressive renal dysfunction) then reduce or discontinue other drugs without proven mortality benefit (namely digoxin, diuretics, calcium channel blockers, amiodarone)
- Diuretics are used to control fluid overload but the goal is to use the minimum effective dose. These drugs can sometimes be discontinued once the patient is asymptomatic
- An effective diuretic dose reduction is more often achieved after ACE-I and BB reach target doses
- By using the minimum effective diuretic dose, it is more likely that symptomatic hypotension and/or unacceptable increases in Cr with ACE-I or BB can be avoided
Aggressive Management of Cardiovascular (CV) Risk Factors (hypertension, diabetes, dyslipidemia, smoking, obesity) and other comorbid conditions is recommended:
- ASA 81 mg daily for patients with CV risk factors or established atherosclerosis
- Treat comorbidities and risk factors as per current guidelines
11. Indications for Referral to a Medical Specialist
- Cause of heart failure unknown
- Suspicion of ischemia or valvular disease as the primary cause
- Severe heart failure that is refractory or difficult to control
- Symptomatic arrhythmias
- LVEF≤ 35% (consideration of cardioverter-defibrillator implantation)
- Consideration for heart transplantation/implantable defibrillator/cardiac resynchronization
- Serum sodium <132 mmol/L (persistent after water restriction)
- Refer to a Nephrologist when renal function is impaired and/or deteriorating and the reason is not apparent (see chronic kidney disease guidelines)
- Refer to the Heart Function Clinic, Cardiac Rehabilitation or Risk Reduction Centre, and to a local Chronic Disease Management Program where available
- Refer to a Geriatric Medicine Specialist or to Long-Term Care Managers when an elderly patient has significant medical comorbidity, medication management issues, and/or significant cognitive, psychological and functional issues
- Advanced Practice Nurses provide integral specialist support of cardiac care in HF clinics where they provide nursing case management for ongoing surveillance and education of patients and family members
12. Heart Failure in the Elderly
- Elderly patients constitute one of the largest groups of patients with HF
- In general, HF medications are under prescribed despite the fact that this group derives a greater absolute benefit from these medications
- Treatment strategies in the elderly patient with HF are the same as other groups. However, care must be taken with respect to medication initiation and uptitration
- A gentle strategy to maximize long-term adherence is preferred because of the propensity for adverse events in this group (especially postural hypotension and digoxin toxicity)
- Assess for relevant comorbid conditions, such as cognitive impairment, that may affect treatment, adherence, follow-up and prognosis
- Identify a capable caregiver
- Consider referral to a specialist in geriatric medicine and/or community support staff
13. Management of Heart Failure with Comorbid Conditions
13.1. Chronic Kidney Disease
- HF patients with stable renal function (Cr < 200 µmol/L and eGFR >30 mL/min) should receive standard therapy with an ACE-I, ARB or spironolactone (use digoxin with extreme caution)
- Monitor serum Potassium (K+) and Cr levels more frequently, especially with combination therapy or in the case of an acute intercurrent illness
- HF patients with persistent volume overload or deteriorating renal function should be assessed for reversible causes - medications (especially NSAIDs), hypovolemia, hypotension, urinary tract obstruction or infection
- Stable oliguric HF patients - daily evaluation of the dose of diuretics, ACE-I, ARB, spironolactone and non-HF drugs that impair renal function is recommended (preferably as an inpatient)
- Stable non-oliguric HF and Cr increase >30% from baseline - consider reducing the dose of diuretics, ACE-I, ARB and spironolactone until renal function stabilizes
- Referral to a Nephrologist is encouraged when there is kidney impairment as defined by a Cr increase of >30%, an eGFR <30 mL/min or eGFR <45 mL/min if cause is unknown
13.2 Anemia (hemoglobin <110 g/L; generally symptomatic if <90 g/L)
- Investigations and treatment should be directed at the underlying cause
- Substrate deficiencies should also be replaced (iron, vitamin B12 or folate)
- There is no evidence to support the use of erythropoietin (or darbepoietin) in HF
- Consider blood transfusion if, after substrate deficiencies have been corrected, anemia and advanced symptoms persist
14. Management during Intercurrent Illness
- During acute intercurrent illness (i.e. pneumonia, COPD exacerbation) BB, ACEI and ARBs should be continued at their usual dose unless they are not tolerated
- If there is a concern about their use, then the dose can be halved during the illness and then uptitrated rapidly as soon as safely possible
- Only with a life-threatening complication should BB, ACEI and ARBs be discontinued abruptly
- HF patients with acute dehydrating illness should have prompt evaluation of their renal function and electrolytes even if they are not overtly volume depleted or overloaded
- If renal function worsens, adjust doses of diuretics, spironolactone, digoxin, ACEI, ARB as necessary
- If surgery is required, then patients with HF should be evaluated by a Physician experienced in HF management perioperatively
- If a patient with HF develops a gout exacerbation, the preferred treatment would include oral colchicine ± prednisone; avoid NSAIDs due to their role in exacerbating HF. Gout can be prevented with the use of allopurinol and/or a reduction in diuretic dose (as tolerated)
15. Ongoing Management
Comprehensive HF management is based on setting treatment goals and monitoring the effectiveness of management:
- Define and monitor cardiovascular goals and the key clinical indicators using a systematic approach (e.g. electronic medical record, flow sheet, file cards)
- Reverse congestion
- Control arrhythmia and ischemia
- Prevent emboli
- Stabilize vital signs (pulse, sit/stand blood pressure, weight)
- Use current drug and non-drug therapy for HF and for cardiovascular and non-cardiovascular comorbidity
- Review medications for intended and unintended effects (inappropriate polypharmacy, potential drug interactions, inadvertent aggravation of comorbid conditions)
- Monitor serum biochemistry (electrolytes, Cr/eGFR) over the short-term (days to two weeks) if the clinical condition or medications have changed . The frequency will depend on whether the current values are normal or abnormal and whether the patient continues to worsen or improve. When stable, remeasurement at six month intervals may be sufficient but will depend on clincal stability and changes in medications
- Monitor serum digoxin only if toxicity is suspected or for checking adherence
- Monitor and treat psychosocial consequences (i.e. non-compliance, anxiety, depression, fear, delirium, dementia, social isolation, home supports and need for respite care)
- Define and re-define the goals of treatment over time with the patient
16. Prognosis of Heart Failure
Outcomes in heart failure are highly variable and it is important to provide accurate information to patients about prognosis to enable them to make informed decisions about medications, devices, transplantation and end of life.

Poor prognostic factors include:
- Recurrent hospitalization for acute HF
- Advanced age (>75 years)
- Female gender
- Ventricular arrhythmias (non-sustained ventricular tachycardia) and atrial fibrillation
- NYHA HF Classes 3 and 4
- LVEF (<35%) or combined systolic and diastolic left ventricular dysfunction
- Marked left ventricular dilatation (LVEDD > 70 mm)
- High BNP levels (See Table 1) - use of BNP for prognostication requires further study
- Low-serum sodium (< 132 mmol/L)
- Hypocholesterolemia
17. Palliative and End-of-Life Care
Predicting time of death in HF is challenging given the cyclical nature of the disease. Helpful clinical prediction tools have been established. Discussions regarding end-of-life care should be initiated with patients who have persistent NYHA Class IV symptomatology or an EF < 25% despite maximal medical therapy (at target doses of study drugs as mentioned above).
Prior to initiating end-of-life care ensure that:- All precipitating factors have been addressed including:
- Residual angina and hypertension
- Adherence to salt and fluid restrictions
- Adherence to medications
- Contributory conditions (arrhythmias, anemia, infections, thyroid dysfunction)
- All active therapeutic options have been appropriately considered:
- The patient is taking maximal medical therapy (target doses of study drugs)
- Biventricular pacing (possibly indicated with QRS > 120 ms)
- Implantable defibrillator (possibly indicated with LVEF < 30%)
- Revascularization (percutaneous intervention or bypass surgery)
- Transplantation options have been explored
- Support of dying patients and their families
- Caregivers should be consulted to determine their degree of burden
- It is important to ensure that advance care planning has been carried out, including financial and health care decisions (e.g. Representation Agreement)
- Control of pain and other symptoms
- Symptoms related to volume overload:
- Adequate diuretic use (sometimes more than one agent) is important
- ACE-I dose may need to be reduced if limited by symptomatic hypotension and renal impairment (Cr > 250 µmol/L or > 30% from baseline)
- Consider choice and dose of narcotic as renal function is likely impaired – i.e. Hydromorphone for narcotic naïve, Duragesic patch. → Consider home oxygen (See COPD Guidelines for indications)
- Decisions on the use of life-sustaining therapies
*Images provided by Microsoft Clip Art
Appendices
Appendix A - DiureticsAppendix B - Beta-Blockers (BB)
Appendix C - ACE-Inhibitors (ACE-I)
Appendix D - Angiotensin Receptor Blockers (ARBs)
Appendix E - Direct-Acting Vasodilators
Appendix F - Spironolactone
Appendix G - Digoxin
Figures
Appendix A - Diuretics
Rationale
- Used to control symptomatic volume overload
Beneficial Subsets
- NYHA class II-IV with fluid overload (edema, ascites, weight gain)
Goal/Dose
- Start with furosemide 20 mg/day and increase/decrease as needed
- Divide the doses BID if > 80 mg/day are required
- Aim for minimum effective dose to control symptoms of fluid overload
- If volume overload persists despite optimal medical therapy and progressive increases in furosemide dose (i.e. >120 mg BID) consider:
- Changing furosemide to bumetanide as oral absorption may be improved
- Cautious addition of metolazone 2.5-5 mg 30 min prior to furosemide dose
- Start with a test dose 3 times/week, closely monitoring daily weight, as well as serum K+ and Cr/eGFR
- Note: Diuretics can be stopped once fluid overload resolves
Monitoring
- Check serum Cr, Sodium (Na+) and K+ before initiating therapy and one to two weeks after each dose adjustment
- Watch K+ carefully: maintain K+ between 4.0-5.5 mmol/L
- K+ may increase when using K+ sparing diuretics (spironolactone, triamterene, amiloride), especially when combined with an ACE-I or ARB
- K+ may increase when K+ depleting diuretics decreased/discontinued while patient on K+ sparing diuretic, ACE-I and / or ARB
- K+ may decrease when using K+ depleting diuretics (furosemide, metolazone, hydrochlorothiazide)
Dealing with Side-Effects
- If Cr increases > 30% from baseline, reduce/hold diuretic until volume status normalizes
- If muscle cramping occurs, check magnesium and calcium and replace as necessary
- If nocturia is a concern, avoid diuretic therapy after 2 pm

Appendix B - Beta-Blockers (BB)
Rationale- BB are the most recent dramatic advance in HF medical treatment
- They slow disease progression, decrease hospitalization, decrease mortality and improve quality of life but have little effect on exercise duration
- All patients with chronic, stable HF (volume controlled NYHA Class I-IV)
- Start when there is no physical evidence of fluid retention (i.e. euvolemic), with a heart rate > 60 bpm and a systolic BP > 85 mmHg
- Not to be initiated in volume overloaded, acute or highly symptomatic HF
- Contraindicated in patients with reactive airway disease (asthma) but can be used for patients with COPD, peripheral vascular disease or diabetes
- Monitor blood pressure, pulse rate and HF symptoms with dose adjustments
- Patients may clinically deteriorate over the first 6-12 weeks but persistence is necessary
- Adjustments may be required in the doses of other medication, including diuretics, vasodilators and ACE-I, at least in the titration phase, to increase the tolerance for BB
- Hypotensive effects:
- Consider general measures as above
- Reconsider need for nitrates, Calcium Channel Blockers (CCB), vasodilators and diuretics
- Reassure: Symptoms of dizziness often resolve within 2-4 weeks of titration
- Worsening fluid overload:
- Intensify sodium and fluid restriction and/or increase diuretic dose
- May have to temporarily reduce BB dose until volume control achieved then retry titration (halve dose if serious deterioration)
- Significant bradycardia:
- Obtain an ECG to exclude heart block
- Reduce or eliminate other drugs that also slow heart rate (digoxin, diltiazem, verapamil, amiodarone)
- Reduce dose of BB
- Consider pacemaker support if severe bradycardia or high grade AV block

Beta-Blocker Equivalent Doses
- The effect of BB in HF is not a class effect. It is recommended that patients already on a beta blocker be changed to one of the recommended agents as above
- The following is presented as a rough guide based only on recommended “usual” and “starting” doses. Therefore, it is recommended that patients are followed closely during and after conversion
- The following doses are equivalent to carvedilol 12.5mg BID

Appendix C - ACE-Inhibitors (ACE-I)
Rationale- ACE-Is slow disease progression, improve exercise capacity and decrease hospitalization and mortality
- All patients with HF (NYHA I-IV)
- If baseline kidney function impaired (eGFR <30 ml/min) do not start
ACE-I start hydralazine/nitrate combination and consult a Nephrologist
- ACE-I may cause a deterioration in kidney function and hyperkalemia, so careful monitoring is required during titration phase
- In most situations these drugs can be used successfully with dosage adjustments of concomitant medications
- Check Cr and K+ before initiating therapy and 1-2 weeks after each dose adjustment (sooner for the elderly)
- On stable therapy check Cr and K+ every 3-6 months
- In most situations these drugs can be used successfully with dosage adjustments of concomitant medications ( ie. diuretics, ARBs)
- If Cr increases > 30% from baseline:
- First reduce/hold diuretic for 1-2 days; if no response then reduce/stop ACE-I and consider hydrolyzing/nitrate combination
- When there is uncertainty about the underlying cause of kidney impairment or management thereof, referral to a Nephrologist is encouraged
- Intractable cough or drug-associated rash:
- First ensure that cough is not due to poorly controlled HF
- Stop ACE-I, consider ARB or hydrolyzing/nitrate combination if ARB not tolerated
- Angioedema may occur with ACE-I (may recur with ARB therapy)
 *Target dose used in large CHF trials with clinical endpoints.
*Target dose used in large CHF trials with clinical endpoints.
Appendix D - Angiotensin Receptor Blockers (ARBs)
Benefical Subsets- NYHA Class II-IV
- ARBs are not first-line agents and are reserved for patients intolerant of ACE-I or BB or for patients in NYHA class II and IV HF despite treatment with both ACE-I and BB
- See above - Same as ACE-I
- Note: Angioedema may recur with ARBs

Appendix E - Direct-Acting Vasodilators
Rationale
- Hydralazine and nitrates in combination are effective at reducing afterload and preload with a mortality benefit that is inferior to ACE-I. For this reason ACE-I are generally preferred
- May have greater benefit in patients of African-Canadian descent
- Not associated with renal failure or hyperkalemia
- ACE-I intolerant patients
- Note: Nitrates can also be useful to relieve orthopnea, paroxysmal nocturnal dyspnea, exercise-induced dyspnea or angina (tablet, spray or transdermal patch)
- Hydralazine results in a tachyphylaxis and may worsen myocardial oxygen demand
- Nitrates require a “drug free” interval, usually 12 hours, to decrease resistance
- Hydralazine and nitrates should be used concurrently

Appendix F - Spironolactone
Rationale- Although a K+ sparing diuretic, this drug exerts its beneficial effects in HF through aldosterone antagonism
- Spironolactone decreases mortality and hospitalization and improves symptoms
- NYHA Class III-IV moderate to severe systolic heart failure
- Extreme caution should be used when adding spironolactone to ACE-I and ARBs due to a propensity for hyperkalemia
- Avoid use in patients with renal dysfunction
- Hyperkalemia may develop if K+ depleting diuretic dose is decreased
- Start at 12.5 mg daily and titrate to 25 mg daily as tolerated (>25 mg rarely indicated)
- Check K+, Cr and eGFR at 3-7 days and 1-2 weeks after each dose adjustment
- Gynecomastia is known to occur in up to 5-10% of males
Appendix G - Digoxin
Rationale- Digitalis may improve symptoms, exercise tolerance and quality of life, but it has not been shown to improve survival
- NYHA Class II-III Systolic HF (digoxin has no role in HF with PSF with normal sinus rhythm)
- Digoxin should be used with caution, especially in women and those with impaired renal function
- Usual dose is 0.125-0.25 mg/day through level 0.65-1 nmol/L 8-12 hours post-dose
- As digoxin levels are typically drawn in the morning, digoxin should be dosed in the evening
- Digoxin: Dose will need to be adjusted in the elderly, those with low body mass, those with impaired renal function and those taking amiodarone
- Electrolytes, Cr and digoxin serum concentrations should be obtained 5-7 days after dose adjustments (approximate time to steady-state)
- Note: It may take 15-20 days to reach steady-state in patients with renal dysfunction
- Obtain a digoxin level whenever toxicity is suspected
- The most important toxic effects are life-threatening arrhythmias (e.g. ventricular tachycardia/ fibrillation, complete atrioventricular block)
- Other symptoms include nausea, vomiting, anorexia, diarrhea, confusion, amblyopia, and, rarely, xerophthalmia may occur
- Note: If hypokalemia or hypomagnesemia (often due to diuretic use) is present, even lower doses and lower serum levels can cause toxicity
Figures


Patient Management
Care Protocols
Care protocols, like medical and nursing procedures, allow staff to offer a consistent approach to managing clinic patients. Care protocols will allow caregivers to establish routines and govern tasks that are performed in the HF clinic as well as tasks that involve other hospital departments and outside agencies. Protocols ensure that key steps are taken to fill potential gaps in the system of care as the patient moves from clinic to hospital or from hospital to clinic.
The development of the following protocols may assist in enhancing the overall management of clinic patients:
- A protocol for patient referrals, which would involve two sub-protocols: one for patients who are referred for medical assessment, another for patients who are referred for patient education
- A protocol for discharge from hospital: this protocol would stipulate that a patient is either seen at discharge or at the clinic within 5 working days, or a telephone follow-up 2 days post-discharge will occur. This protocol should also describe clearly the sequence of events that occurs after discharge to ensure patients understand their care path
- A clinic notification protocol to outline when a patient has contacted the clinic about problems, and how those problems were dealt with. Guidelines for dealing with urgent vs. non-urgent calls
- A protocol for discharge from the clinic
Data Collection
Recent data suggest that, despite medical intervention, HF mortality remains high at a time when morbidity and mortality rates from other common cardiovascular diseases (such as myocardial infarction) are on the decline. Many heart failure patients experience frequent acute medical crises resulting in high hospital readmission rates and increased health care costs.
There is an urgent need to reduce mortality and morbidity associated with HF, reduce hospital admissions and readmissions, and improve patient management. HF clinics have been shown to be an effective alternative to inpatient management of this patient population.
Data collection, using a standard data-gathering tool, will allow practitioners to review and change practice patterns to enhance patient care and improve the quality of life for HF patients and their families.
In general, data collection will allow practitioners to monitor patient issues, measure clinical outcomes, track public health data, document the need for a HF clinic, secure clinic funding, and answer research questions.
Care Plan
A patient care plan, which specifies interventions and teaching done by staff and the anticipated patient outcomes, should be initiated and followed on all patients.
Such a care plan will ensure that patients receive optimum care and understand all facets of their diagnosis and long-term care. Care plans should be customized to meet the individual needs of each patient and should be developed with input from patients and family members.
Moreover, a care plan enhances communication and ensures continuity of care.
*Draft changes pending adoption by CHFNStarting a HF Clinic
Assembling the Team
At a minimum, team members starting a multidisciplinary HF clinic should consist of:
Executive SponsorThis person should be a member of the hospital executive who give the clinic the “rubber stamp” of approval and who will advocate on the clinic’s behalf.
Administrative Leader
The administrative lead should have the ability to hire staff, ensure the day-to-day operations are in order, provide support where needed and arrange for appropriate space and resources.
Physician Leader with expertise in HF Care
The Physician should provide clinical leadership as well as active involvement in preparing the protocols and pathways required for good patient care. The Physician should be committed to providing this leadership.
Nurse(s) with skills in heart failure and patient teaching
Within the multidisciplinary model, the Nurse should have extensive cardiac experience, specifically in HFcare. The Nurse should have skills in education and understand the concepts of chronic disease management.The level of nursing support decided upon may vary from clinic to clinic. Some clinics prefer the Nurse Practitioner role, others an expert Registered Nurse and others a hybrid of both roles. This is a decision that needs to be made with the team from the outset. Nurse Practitioners can provide a wider scope of care, whereas the registered nurse can practice with Physician orders. The scope of practice varies between provinces and we recommend that this is ascertained before starting.
- Able to provide heart failure self-management teaching and support
- Advanced cardiac assessment skills
- Confidence to introduce the concept of end of life planning
- Safely provide telephone support/advice to patients
- Able to use word processing, email, and spreadsheets on computer
The Clerk should be responsible for making appointments, registering the patients, phoning patients before the clinic, filing, preparing charts for the visit, taking calls, collating lab and test results for checking by the Physician/Nurse Practitioner.
Programs with the following resources should also consider support from the following health care providers:
- Pharmacist
- Dietitian
- Physiotherapist
- Social Worker
- Palliative Care
- Geriatrician
- Palliative Care
- Occupational Therapist

Staffing Levels
It is not easy to determine staffing levels. First, it is important to determine how many patients the clinic may expect. To do this, data around local HF demographics should be sought and a clear care pathway be defined to ensure that once the endpoint is reached that the patient is discharged back to their referring source.
A survey to determine patterns of staffing in heart function clinics across Canada was performed in 2004 (presented at Canadian Cardiovascular Congress, 2004 by Kaan A, Clark C and Edmonds M). Fifteen clinics responded and showed that:
- Most clinics (87%) function using the “Nurse-managed, Physician-directed” model of care. Meaning that the day to day function of the clinic is managed by the Nurse, however the care of patients is directed by the Physician. One clinic was directed by a Nurse Practitioner. As this survey is now 6 years old, this model may have changed somewhat
- 40% of clinics see 10-19 patients per week. There was great variation in the number of patients seen as some clinics were just one session per week and some ran 5 days per week
- On average, clinics see 8 patients per session
- Average caseload of RNs was 136 patients (range 60-200). One Nurse saw 10 to 20 patients per week
- One Clerk manages an average caseload of 50 patients per week
- 25% of nursing time involved clerical duties and data entry, the rest was telephone support, clinic visits and patient education
There must be a commitment to meet regularly to assess staffing levels based on the patient load and whether or not the patients are appropriate for the clinic.
Developing a Clinic Philosophy
The philosophy of the HF clinic should be spelled out early on. What is it that the clinic wants to achieve? This focuses the team and allows for planning of services.
Identifying Key Indicators
It is important to identify what indicators the clinic will measure to determine success and monitor progress. The CHFN recommends the following indicators: symptoms, quality of life, heart function, HF hospitalizations, CV hospitalizations, and survival.
Measuring Outcomes
Membership to the CHFN facilitates access to the National Database. For more information on applying for membership please go to https://www.chfn.ca/how-to-become-a-chfn-site. Each new centre needs to have:- A Physician leader of the HF clinic
- A commitment to HF management and follow up
- A Nurse (full or part time) with special expertise and training in HF management
- A sufficient number of HF patients and referral community
- A commitment to enter their patient data into the database with regular downloads to national database
- A willingness to sign a contract of agreement.
The database is designed as a local tool like an electronic medical record but also allows download of data without specific patient identifiers to the National Database. The data that is uploaded is secure and password protected, as the upload technology uses the same encryption technology used for online banking. All patients must sign a consent form before their unidentified data can be entered into the database and uploaded to the national database. There is a consent template located in the members section. Once we have approved and received your signed Program Agreement, you will get a username and password for the website.
Support
What we can give to you is the database to help organize and track your patients locally (you ‘own’ this data), opportunity to benchmark your clinic with the National data, opportunity to ask research questions of your data and that of the National data, use of the data to lobby more effectively for local resources, an invitation to come to our annual meeting currently held in conjunction with the Heart Failure Society of America in September, networking with like minded colleagues to improve the management of HF patients and to learn together, and access to all benefits of the website and the Network.
Team Development
The clinic should meet each month at least to review difficult cases, prepare a plan and to review clinic issues. An agenda should be prepared and action items prepared. Once a year, it is valuable for the team to meet in a “retreat” style to review outcomes, revise the goals and plan for the year. The CHFN database is able to provide centre specific reports that allows a program to track outcomes.
Documentation
Some sample documentation is included that may help with preparing local documentation:
Patient Education
Introduction
Patient education is one of the most important functions of a heart failure clinic, and is the key to the success of a HF management program. Education should involve all members of the multidisciplinary clinic team and must be ongoing.
Health Professional Patient Education
Introduction
 Patient
education is one of the most important functions of our heart failure
clinics. This education comes from all members of the
multidisciplinary clinic team responsible for your care and is
ongoing.
Patient
education is one of the most important functions of our heart failure
clinics. This education comes from all members of the
multidisciplinary clinic team responsible for your care and is
ongoing.
This section presents a brief overview of state-of-the-art clinical information for health professionals who care for health failure patients. There are six (6) educational sections. You may use this section as a review for yourself prior to patient teaching. In additional, the eight (8) patient information sections allow you to teach directly from the pages.
Members of CHFN may wish to use the information provided as a reference tool and use a flip chart or other medium to share the information with patients and their families. The patient information sheets are also supplied as information pads that are numbered for each section/topic. Members may distribute the sheets following each educational intervention:
Pathophysiology of Heart Failure
'Chronic Heart Failure' or 'Congestive Heart Failure'?
The word “congestive” means different things to different people and leads to a great deal of confusion. Overall, it is better to discuss “heart failure” with your patients. Different kinds of heart failure include:
- Acute heart failure
- Chronic heart failure
- Systolic heart failure
- Diastolic heart failure
- Left ventricular heart failure
How the Normal Heart Functions
The heart is a hollow muscle about the size of a fist. A normally functioning heart is one of the strongest muscles in the human body. It pumps blood through the lungs to deliver oxygen to the remainder of the body.
The heart is divided into four cavities: two atria and two ventricles. The left atrium receives oxygenated blood from the lungs. From there, the blood passes to the left ventricle, which pumps it via the aorta through the arteries to supply the tissues of the body. The right atrium receives the blood after it has passed through the tissues and given up much of its oxygen. The blood then passes to the right ventricle, and then to the lungs, to be oxygenated. The heart tissue itself is nourished by the blood in the coronary arteries.
Definition of Heart Failure
Heart failure (HF) is a state in which the heart is unable to pump blood at a rate that meets the requirements of metabolizing tissues or can do so only from an elevated filling pressure.1
The incidence of heart failure rises with increasing age, and is three times more likely to occur in men than women. Analysis of numerous published studies indicates that the incidence of heart failure is between 2.3 to 3.7 per thousand per year.2
Usually, HF manifests initially during exertion, however, as the disease progresses the contractile performance of the heart deteriorates and shortness of breath and fatigue result, even when the body is at rest.
Etiology of Heart Failure
The two main causes of HF are:
- Myocardial infarction, with loss of heart muscle secondary to coronary artery disease
- Chronic hypertension
Heart failure can also result from:
- Viral infection of the heart
- Valvular disease
- Alcoholism or other toxins
- Congenital conditions
- Acquired immunodeficiency syndrome
Heart failure can be aggravated by:
- Diabetes
- Anemia
- Thyroid disease3
| Left heart failure (low output/pulmonary congestion) |
Right heart failure (systemic venous congestion) |
| • Dyspnea • Orthopnea • Paroxysmal nocturnal dyspnea • Fatigue • Cough |
• Peripheral edema • Weight gain • Anorexia • Abdominal discomfort • Fatigue |
These symptoms may be accompanied by:
- Angina
- Cool extremities
- Tachypnea
- Tachycardia
- Elevated jugular venous pressure
- Positive hepato-jugular reflux
- Rales, wheezes
- Added heart sounds
- Pleural effusion
- Detection of enlarged heart on x-ray4
References
- Colucci W, Braunwald E. Pathophysiology of heart failure. In: Braunwald E, ed. Heart disease. 5th Edition. Philadelphia: WB Saunders, 1997;394-420.
- Cardiology Preeminence Roundtable. CHF in Brief. In: Beyond four walls: research summary for clinical and administrators for CHF management. Washington D.C.: The Advisory Board Company, 1994.
- Adams KF, Zannad F. Clinical definition and epidemiology of advanced heart failure. Am Heart J 1998;135(Suppl 2, Part 6):S204-S215.
- Canadian Cardiovascular Society. Report on the 1993 Consensus Conference on the Diagnosis and Treatment of Heart Failure. Guidelines for the management of heart failure. Toronto: Publications Ontario, 1996.
Dietary Considerations
The relationship between proper nutrition and control of heart failure is well understood: low salt intake, reduced alcohol consumption, and a well-balanced diet are the mainstays of helping patients manage HF.1
When discussing diet and nutrition, it is important to involve the patient’s spouse, family members, and caregivers. In many cases (particularly with men) HF patients are not the primary food preparer in the household and may be unaware of the caloric, salt, and fat content of the foods they’re ingesting. In cases where a patient’s diet must change, involving their family in these changes will promote compliance.
Canada’s Guide to Healthy Eating offers an excellent template for counselling patients about diet. Encouraging patients to eat foods from the four major food groups will ensure they get their daily requirement of essential nutrients and vitamins.
All heart failure patients should receive written dietary guidelines, reinforced orally by the clinic nurse during regular clinic visits. Those with limited reading ability and certain ethnic groups with unique food preferences should receive specialized counselling.1
Lowering Sodium Intake
Sodium intake should be limited in patients with HF because it is
not efficiently excreted
from their system. In patients taking diuretics, the drug is rendered
less effective
when sodium intake is not limited.2
The average person requires less than 500 mg/day of sodium, however, most consume between 5-6 grams/day. The optimum daily salt intake for HF patients is 2 grams/day or less, however, some patients find their diet unpalatable at this level. Therefore, depending on their stability, this level of sodium intake may be increased to 3 grams/day.1 Patients taking large amounts of diuretics (>80 mg/day of furosemide) need to maintain their sodium intake at 2 grams/day or less. However, for patients with mild to moderate, stable heart failure without fluid retention, 3 grams/day is a reasonable target.1
In order to increase compliance with a low-sodium diet, patients should be advised to:
- Stop using the salt shaker (remove it from the dinner table)
- Not add salt to food during preparation
- Read food labels carefully
- Stop eating processed and high-sodium foods: the greatest source of sodium (up to 80%) is the salt and other sodium compounds added to food during processing
- Be aware of ‘hidden’ sources of sodium: for example, one slice of bread contains only 150 mg of sodium, however, the quantity of bread eaten during one day could cause total daily sodium intake to be high
Assessing your Patient’s Sodium Intake/Setting Goals for Reduction
Questions that will help assess your patients’ sodium intake are:
- Who prepares your food?
- Is salt added during food preparation?
- Do you add salt to your food at the dinner table?
- How much bread do you eat?
- How often do you eat in restaurants?
- Do you request that your food be prepared without salt or monosodium glutamate?
- How often do you eat processed food (frozen dinners, canned soups, salad dressings, luncheon meats, cheese)?
To ensure compliance with a reduced-salt diet, set small, incremental, achievable goals with your patients (i.e. cut out salt during food preparation, take the salt shaker off the dinner table, stop eating fast food or prepared food). To give patients ‘control’ over their health care, allow them to prioritize the changes they need to make, but help them determine which actions will have the greatest impact on lessening sodium in their diet.
Use this chart to discuss common foods and their sodium content:
|
Alcohol
Acute ingestion of alcohol depresses myocardial contractility in patients with known cardiac disease. If alcoholism is the suspected cause of a patient’s HF, alcohol intake should be strongly discouraged. For patients with Class I or II HF, ingestion of alcohol should not exceed one drink per day, i.e. 30 mL of liquor, or its equivalent in beer or wine.1
Smoking
Abstinence is recommended for all patients, especially those with ischemic heart disease (IHD).2
Fluid Restrictions
Unstable HF patients should ingest no more than 1 litre of fluid per day. The recommended daily intake for stable HF patients is 2 litres, which is equivalent to about 6 glasses of water. However, patients must be counselled that not all fluid intake comes from drinking liquids, and that fluid contained in foods such as fruit or soups must be factored into their daily calculation.2
Daily Weigh-in/Weight log
Patients’ weight should be taken and recorded during every clinic visit, to determine whether it has remained stable or if they are experiencing undue water retention. Patients should also be encouraged to weigh themselves daily – particularly if they are taking diuretics – to monitor their weight. Specific instructions to patients include: weigh yourself after emptying your bladder, before breakfast, every morning, wearing the same type of clothing, and using the same weigh scale.
Patients must be counselled to seek medical help immediately should they gain or lose weight quickly. A daily weight log will help monitor weight and encourage control over drug (diuretic) therapy.
Vitamin Supplementation
Vitamin supplementation may be considered for severe HF patients, since vitamin loss may occur with marked diuresis.1
References
- Dracup K, Baker D, Dunbar SB, et al. Management of heart failure: counselling, education and lifestyle modification. JAMA 1994;272:1443-1446.
- Uretsky BF, Pina I, Quigg RJ, et al. Beyond drug therapy: nonpharmacologic care of the patient with advanced heart failure. Am Heart J 1998;135(Suppl 2, Part 6):S264-S284.
Exercise
Until recently, exercise was contraindicated in patients with HF. However, lack of activity may have long-term detrimental effects on physical functioning. Numerous studies have shown that patients with HF can safely engage in suitable physical activity and improve their exercise capacity.1 In fact, one recent study suggests that higher levels of activity are associated with increased levels of functioning and wellbeing for patients with chronic HF.2
While stressing the seriousness of your patient’s illness and disease progression, you can also encourage an exercise plan that enables them to remain active and enjoy a reasonable quality of life.
Unfortunately, many patients diagnosed with HF were overweight and inactive prior to development of the disease. As a result, it can be a challenge to initiate an appropriate exercise program to which patients will adhere.
The functional classifications of heart failure can serve as a guide to determine the safest level of activity for your patients:
| Class I: | No limitation of physical activity. Exercise for 30 minutes or longer. |
| Class II: | Slight limitation of physical activity. Most physical activity needn’t be restricted, however, ordinary exercise may result in fatigue or dyspnea. |
| Class III: | Marked limitation of physical activity. Ordinary forms of exercise should be moderately restricted. The patient may only be able to walk 10 minutes per day. |
| Class IV: | Severe limitation of physical activity. Any strenuous activity can increase discomfort and result in shortness of breath or angina. |
Helping your Patients Establish Realistic Exercise Goals
- Assess your patient’s current level of physical activity by
asking the following questions:
- How many blocks can you walk before getting short of breath or fatigued?
- Are you breathless with minimal exertion, or when you wake up?
- Do you have chest discomfort when walking?
- What type of activity do you enjoy now? In the past?
- Involve your patients in the management of their diagnosis and empower them to take responsibility for their well-being.
- Assist your patients in developing a regular, progressive exercise program that will help them to increase their endurance gradually, at their own pace.
Tips for Discussing Exercise with your Patients
Explain the benefits of exercise:
- Improved muscle strength and tone
- Reduced effects of osteoporosis
- Improved functional capacity
- Improved quality of life
Determine Appropriate Exercise Programs for your Patients
- Move from simple to complex: for example, start walking one block per day, assess for symptoms, and then increase distance accordingly
- Increase amount and type of activities according to symptoms: housework, gardening, grocery shopping, or social activities can be initiated and then assessed for symptoms
- Initiate other activities based on patients’ preferences and tolerance, such as swimming, golfing, etc.
Specific Tips for Increasing Physical Activity
- Exercise for short periods throughout the day
- Do not exercise directly after eating
- Make exercise part of a daily routine (i.e. walking each morning to get a newspaper)
- If persistent shortness of breath, chest pressure, or pain occurs, contact the CHF clinic
Tips for Exercise Safety
- Encourage warm-up and cool down exercises
- Encourage a small amount of exercise at frequent intervals, instead of trying to do too much all at once
- Discourage sudden, unexpected changes in physical activity levels
While stressing the importance of physical activity, reinforce the necessity of resting and storing energy as well. Patients should be counselled to:
- Alternate several periods of rest with exercise or other activities during the day
- Use various methods of resting, such as reading, watching television or napping
- Use equipment to save energy, such as bathtub chairs, etc.
- Elevate their legs during rest periods to avoid swelling
Sexual Activity
Fears about physical exertion may contribute to the high prevalence of sexual dysfunction reported in HF patients.1 While there is frequently reluctance or embarrassment when discussing it, HF patients need to know how to approach sexual relations in light of their diagnosis. Although sexual practices may need to be altered in patients with limited exercise tolerance, there is no reason they need to be curtailed completely. Generally speaking, patients can continue their normal sexual activities, but should be counselled not to have sex if they’re tired, tense, or have just completed a strenuous activity.
Because discussing sex is such a sensitive issue, do not expect your patients to raise it – clinicians must be prepared to introduce the subject in a frank and supportive manner.
References
- Dracup K, Baker D, Dunbar SB, et al. Management of heart failure: counselling, education and lifestyle modification. JAMA 1994;272:1443-1446.
- Stewart AL, Hays RD, Wells KB, et al. Long-term functioning and well-being outcomes with physical activity and exercise in patients with chronic conditions in the medical outcomes study. J Clin Epidemiol 1994;47:719-730.
Medications
A variety of medications may be prescribed for HF patients. The following information will help health professionals to fully inform patients of each drug’s mechanism of action and clinical effect.
Patients should be educated that maintaining a relationship with only one pharmacist will help ensure better continuity of care.
Angiotensin Converting Enzyme (ACE) Inhibitors
Patients with HF have enhanced renin-angiotensin-aldosterone system activity, resulting in elevation of angiotensin II, which promotes sodium and water retention. ACE inhibitors work by decreasing the production of angiotensin II, which then results in improved hemodynamic function in HF patients. Numerous clinical trials have indicated that ACE inhibitors have a major impact in all stages of HF.1
Recent studies have also found that ACE inhibitors have a favourable effect on ventricular remodelling and coronary vascular events. ACE inhibitors have also been shown to reduce hospitalizations and improve survival in HF patients who have had a myocardial infarction and in those with chronic LV dysfunction. In fact, ACE inhibitor therapy has been shown conclusively to reduce mortality and morbidity in HF patients.2
However, concerns about the side effect profile of ACE inhibitors (frequently unjustified if the drug is properly used) render them underused by many practitioners. Common side effects include change in renal function and development of hypotension with dizziness, cough, or both. Other side effects include skin rash, upper abdominal pain, headache, mental confusion, uremia, acute renal failure (in patients with renal artery stenosis), impotence, and, rarely, angioneurotic edema.
Beta-Adrenergic Blockers
Beta-adrenergic blocking agents have been shown to reduce heart rate and improve heart function in HF patients. Recent studies report improved survival, reduced hospitalization, and reduced rates of worsening heart failure rates in stable HF patients introduced to beta-blockers.3,4
Once patients are started on beta-blockers, careful follow-up is crucial. Alteration in accompanying therapies will also be necessary (increase in diuretic dose, for example). Beta-blockers may be useful in patients with atrial fibrillation and have been shown to produce a rapid ventricular response in patients with a high sympathetic tone that prevents rate control with digoxin alone.1
However, beta-blockers may lead to worsening heart failure before improvement is seen. LVEF tends to worsen initially in response to beta-blockers, but subsequently improves after 6-12 months of therapy, an improvement in LVEF not seen with other heart failure medications.1 Low doses must be used initially and then gradually increased over weeks to months.
Diuretics
Diuretic therapy plays a crucial role in both acute and chronic management of HF. The administration of diuretics to patients with HF results in a fall in peripheral vascular resistance and an increase in venous capacitance as well as diuresis. There are three main classes of diuretics: thiazides, loop diuretics and potassium-sparing agents.
Introduced clinically in the 1950s, the major effects of thiazides are to increase sodium chloride and water excretion together with an increase in potassium excretion. Thiazides are rapidly absorbed and diuresis may begin within one hour after oral administration. In patients with decreased renal function, thiazides are relatively ineffective.5
Loop diuretics inhibit sodium chloride reabsorption and augment water excretion. In patients with compromised renal function, loop diuretics are preferred. Loop diuretics are quick acting (30-60 minutes after oral administration and 2-5 minutes after IV administration). For patients with recurrent fluid retention, a twice-daily dose of a loop diuretic (furosemide up to 120 mg BID, 5 mg bumetanide BID, or 200 mg ethacrynic acid BID) is indicated. Higher doses can be considered in individual patients.
Potassium-sparing agents inhibit sodium reabsorption and cause moderate natriuresis. Their major action is to cause potassium conservation and retention.5 They are usually used in combination with thiazides or loop diuretics in CHF patients. It is important to remember that ACE inhibitors can cause potassium retention. Because of this, patients taking ACE inhibitors and potassium-sparing agents should be monitored carefully.
Spironolactone (25-50 mg OD) has recently been shown to improve survival in NYHA Class III-IV HF patients when used in combination with ACE inhibitors.
The end point of diuretic therapy is relief of symptoms, development of orthostatic changes in blood pressure, or a progressive increase in blood urea nitrogen and creatinine.5 The dose of diuretic may be decreased to allow for upward titration of ACE inhibitors.6
Digitalis/Digoxin
Digitalis has been used for centuries in the management of HF. It is extracted from the dried leaves and seeds of the foxglove plant. At least 90% of digitalis therapy in North America is carried out with digoxin.7 Digoxin is a positive inotrope that also decreases sympathetic activation. In patients with HF and regular sinus rhythm, digoxin improves hemodynamics at rest and during exercise.
Discontinuation of digoxin leads to worsening of HF symptoms and decreased exercise tolerance. This is associated with a reduction in ejection fraction and increase in heart rate.7
In the DIG (Digitalis Investigation Group) trial, digoxin had no benefit on survival but reduced symptoms and hospitalizations due to worsening heart failure.8
Nitrates and Hydralazine
Nitrates and hydralazine are indicated in patients who cannot tolerate ACE inhibitors or who have a contraindication to their use. Nitrates alone may also be beneficial in HF patients, however, hydralazine alone has not been shown to be beneficial. The combination is used as adjunctive therapy to digitalis or diuretics.
Angiotensin II Receptor Antagonists
This class of drugs holds considerable promise for heart failure patients, but their role is still to be defined. At present, they are indicated if a patient cannot tolerate ACE inhibitors. It should be noted, however, that renal dysfunction is as likely to occur as with ACE inhibitors.
Anticoagulants and Antiplatelets** (Warfarin and Aspirin)
Warfarin is currently the antithrombotic agent of choice in patients with atrial fibrillation, a history of embolic events, and an ejection fraction of <20%. Warfarin is also effective in preventing thrombus formation in patients at high risk of LV mural thrombosis after myocardial infarction.
Aspirin is indicated for all patients with symptomatic atherosclerotic disease.
Amiodarone
Amiodarone is not routinely used in the treatment of heart failure. However, it is prescribed in heart failure to maintain sinus rhythm and prevent symptomatic, sustained ventricular tachycardia.
Inotropic Agents
Several studies have reported that oral positive inotropic agents are associated with increased mortality rates in HF patients. Consequently, no oral inotropic agents except digoxin should be used in patients with advanced HF.2 Intravenous inotropic agents are currently used for the short-term management of heart failure patients as a bridge to surgery or to stabilize patients with advanced disease.
Conclusions
- ACE inhibitors and beta-blockers should be used in appropriate patients to improve heart function and patient outcomes.*
- Diuretics, digoxin, and nitrates should be considered for symptom relief and to improve signs of heart failure.
* Consult the respective product monographs for appropriate prescribing information.
References
- Gheoghiade M, Cody RJ, Francis GS, et al. Current medical therapy for advanced heart failure. Am Heart J 1998;132:S231-S248.
- The SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992;327:685-691.
- Colucci WS, Packer M, Bristow MR, Gilbert EM, et al. Carvedilol inhibits clinical progression in patients with mild symptoms of heart failure. Circulation 1996;94:2800-2806.
- Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996;334:1349-1355.
- Agarwal R, Ram CVS. Diuretics. In: Cardiovascular Pharmacology and Therapeutics. Eds., Singh BN, Dzau VJ, Vanhoutte PM, Woosley RL. Churchill Livingstone Inc. 1994:353-369.
- Randomized Aldactone Evaluation Study (RALES). Presented at the American Heart Association Meeting [Abstract]. November 1998.
- Packer M, Gheoghiade M, Young JB, et al. for the RADIANCE Study Group. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting-enzyme inhibitors. N Engl J Med 1993;329:1-7.
- The Digitalis Investigation Group (DIG). The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 1997;336:525-533.
**Draft changes pending adoption by CHFN
Patient counselling
Treatment Goals
Patients must be taught that the goal of treatment for HF is to control symptoms. Heart failure usually cannot be cured, however, a patient’s physical condition will stabilize or improve with proper medication and diet.
The term ‘heart failure’ strikes terror in patients, so it must be explained with care and compassion. Such discussions should be governed by the level at which a patient is able to understand the clinical information being imparted, by their desire to learn, and their emotional ability to accept the information.1
The impact of heart failure on a patient’s life is as much related to their psychological outlook as it is to their physical adaptation to the disease. Patients must adjust to the psychological burden of living with new limitations, and the knowledge that their life expectancy may be shortened.2
Factors that Affect Outcomes
During every clinic visit, whether it is acute care or regular follow-up, nurses must offer counselling and education, and monitor patients’ understanding of:
- Medication compliance, and the importance of having all prescriptions filled at the same pharmacy
- Eating a well-balanced diet
- Adhering to a low-sodium diet
- Daily weight-taking
- Getting adequate exercise
- Maintaining a positive outlook on their health
Counselling and Family/Caregiver Support
It is crucial to involve all family members in the care and support of HF patients. By obtaining the involvement of all interested parties, the chances for patient compliance are much greater.
Family-centered intervention is practised in many centres, the goal of which is to empower both patients and their significant others to be part of the health care team. This type of counselling consists of an approach whereby communication patterns within a family are examined and studied, to determine the best way of advising patients to ensure remembrance of and compliance with information that is imparted to them.
It is important also to instill in patients the hope, courage, and inspiration to get through acute episodes and learn to live as normal a life as possible during non-acute periods.
Depression and anxiety are frequent side-effects of HF, in particular, immediately after diagnosis. Nurses must be on the lookout for such behaviours, counsel accordingly when they present, and refer to psychological/psychiatric counsellors when appropriate.
Living Wills/Advance Directives (DNRs)
It is important for the cardiac health care team to understand their patients’ treatment wishes. Since many patients diagnosed with HF are reluctant to discuss advance directives (such as DNRs) or death with family, nurses are in a prime position to initiate discussion and refer them to the necessary resources to assist them. Clergy members and social workers are valuable in helping patients come to terms with their illness and make decisions about how they wish to be treated, as well as helping families participate in this process and support the patient.
Social Work Support
Some institutions retain trained cardiac social workers who can deal with specific needs such as:
- Reviewing the patient’s economic status
- Reviewing the patient’s physical surroundings and lifestyle, and counselling them to make changes if/when needed
- Counselling family members in coping with the patient’s illness
- Directing the patient to home care and other support agencies
- Examining government funding issues, and helping patients complete necessary forms to receive financial assistance
- Helping patients make travel arrangements to attend clinics
References
- Uretsky BF, Pina I, Quigg RJ, et al. Beyond drug therapy: nonpharmacologic care of the patient with advanced heart failure. Am Heart J 1998;135(Suppl 2, Part 6):S264-S284.
- Dracup K, Baker DW, Dunbar SB, et al. Management of heart failure II: counselling, education and lifestyle modifications. JAMA 1994;272:1442-1446.
Follow-up care
Stable Patients
Stable HF patients should be seen at the clinic at regular intervals – every three to six months depending on the severity of the illness. Between visits, certain procedures can be scheduled when required, including interim blood work, checking digitalis levels, and INRs (international normalized ratio).
A viable telemanagement system should be put into place, letting patients know the hours they can telephone the clinic and speak to a clinic nurse for advice and support. A 24-hour pager number should also be publicized for their assistance.
It is very important to communicate clearly with the family and the referring physician so that a proper treatment plan can be implemented and reinforced.
Unstable Patients
Unstable patients must be followed daily or weekly. During clinic visits, the following procedures are done: physical assessments, lab assessments, medication adjustment, compliance monitoring, IV diuretics if necessary, and exercise/activity counselling.
The main aim for unstable patients is to minimize hospitalization. Telemanagement for unstable patients is an important factor in achieving this aim. Clinic staff should be prepared to talk with patients as often as needed to ensure that problems are solved before they become exacerbated.
Providing refrigerator magnets or door hangers with the clinic’s telephone and pager numbers will help to ensure patients have the information they need at their fingertips.
Support groups for both stable and unstable patients provide an excellent opportunity for people to learn from experts and network with others. Moreover, support group meetings allow clinic staff to view and assess patients health status during ‘normal’ activity, instead of only in the clinic setting.
Telephone Support
Patient telemanagement helps nurse specialists track and manage large number of patients. Its aim is to identify early warning signs and correct patient problems before hospitalization for an acute event occurs. Nurse specialists who track and manage patients by telephone should be equipped with computer decision algorithms to assist in problem solving and foster proactive patient management.
In the absence of many other proactive outpatient initiatives, clinics are advised to consider telephone management of HF patients. There is indeed evidence that telemanagement alone can reduce the cost of HF by decreasing hospital admissions and inpatient length of stay when hospitalization is necessary.1
Since many acute HF episodes are linked to noncompliant behaviour or patients’ poor understanding of their symptoms, inadequate patient self-care often goes unnoticed by caregivers who focus on treatment, not health maintenance.1
By telephoning patients regularly at home, clinic staff identify problems, educate, and provide logistical support for patients. Points to cover during telephone follow-up include:
Problem Identification
- Do you have any physical complaints?
- Can you identify any symptoms of deconditioning?
- Have your symptoms worsened or changed suddenly?
Education
- Discuss dietary restrictions
- Reinforce effects of medical noncompliance
- Strongly discourage alcohol use, reiterate benefits of smoking cessation
Logistical Support
- Schedule visits
- Help arrange transportation to clinic, outpatient hospital services
- Make referrals to home care, social services or physicians as needed
The two main benefits of telephone management for patients are:1
- Patients gain access to nurse specialists trained to identify worsening conditions, and to triage appropriate care modality
- Patients living at a distance from hospital need not travel to receive adequate care
References
- Cardiology Preeminence Roundtable. Beyond four walls: cost effective management of chronic heart failure. The Advisory Board Company, 1994.
Helpful Tips for Patients
 Patient education is one of the most important functions of our heart failure clinics. This education comes from all members of the multidisciplinary clinic team responsible for your care and is ongoing.
Patient education is one of the most important functions of our heart failure clinics. This education comes from all members of the multidisciplinary clinic team responsible for your care and is ongoing.
This section presents some basic and easy-to-understand explanations on heart failure for you and your families. A number of handouts and check-sheets are available to help you monitor your medical condition (medications, diet, weight, exercise, hospital admissions, and emergency room visits) and keep health professionals who care for you informed of your progress.
The eight patient information sheets posted below are also supplied as information pads that are numbered for each section/topic. They are available from your clinic team:
What is Heart Failure?
How Does a Normal Heart Work?
 The
heart is a hollow muscle about the size of your fist. It pumps blood
with oxygen and nutrients throughout your body. The heart has four
chambers: two at the top, called atria, and two at the bottom, called
ventricles. The heart is divided into right and left sides. The right
side receives blood from the body and pumps it to the lungs to
increase its oxygen content. This blood is then pumped out to the rest
of the body by the left side of the heart.
The
heart is a hollow muscle about the size of your fist. It pumps blood
with oxygen and nutrients throughout your body. The heart has four
chambers: two at the top, called atria, and two at the bottom, called
ventricles. The heart is divided into right and left sides. The right
side receives blood from the body and pumps it to the lungs to
increase its oxygen content. This blood is then pumped out to the rest
of the body by the left side of the heart.
When you have heart failure, your heart is unable to pump enough blood to satisfy your body’s requirements. Blood that should be pumped out of the heart may back up into other organs or tissues, such as your lungs, stomach, liver, intestines or legs.
What Role Does the Heart Play in the Body?
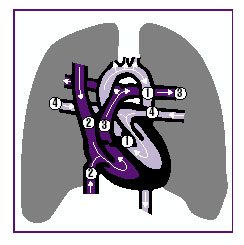 The heart is divided into left and right sides. The left side of
the heart pumps blood rich in oxygen to your muscles, skin, and organs
by means of vessels called arteries. The left side of the heart is
shown in the picture as (1). At the same time
that blood is providing nutrients and giving oxygen to the cells of
your body, it is removing waste matter from these cells. Oxygen-poor
blood, also containing waste matter, then returns to the right side of
the heart through vessels called veins (2).
The heart is divided into left and right sides. The left side of
the heart pumps blood rich in oxygen to your muscles, skin, and organs
by means of vessels called arteries. The left side of the heart is
shown in the picture as (1). At the same time
that blood is providing nutrients and giving oxygen to the cells of
your body, it is removing waste matter from these cells. Oxygen-poor
blood, also containing waste matter, then returns to the right side of
the heart through vessels called veins (2).
From there, the blood is pumped to the lungs (3) where it is
oxygenated and cleaned of carbon dioxide. It then returns to the left
side of the heart through the pulmonary veins (4) so that it may be
repumped throughout the body. Much of the waste matter accumulated
from cells is cleared by the liver and kidneys.
Why do I have Heart Failure?
There are many reasons why you may have heart failure. It can result from:
- A heart attack
- Your heart muscles are unable to pump effectively
- Long-term high blood pressure
- A valve in your heart may not be working properly
- You may have been drinking too much alcohol over a long period of time
- A congenital birth defect
Heart failure can be controlled. In most cases, it cannot be cured.
What are the Symptoms of Heart Failure?
- Tiredness
- Weakness
- Cold limbs
- Loss of appetite
- Swelling in your legs and ankles
- Breathlessness
- A dry, hacking cough
- Waking up from sleep with shortness of breath or feeling smothered when you lie down to try and sleep
What Treatment Will I Receive?
You will probably need to take several different medications, follow a low-salt diet, limit your intake of fluids, and ensure you get plenty of rest, combined with periods of exercise.
Your Diet
Salt Intake
People with chronic heart failure need to maintain a diet low in salt (sodium). Sodium can make your body retain water, which may cause swelling and stress on your heart. You may consume between 2 and 3 grams of sodium per day. It is fairly straightforward to monitor how much salt you eat:
- Do not use the salt shaker at the dinner table. Instead of salt, use herbs, spices, garlic or salt substitutes (just make sure they do not contain potassium chloride, which could be harmful for your heart). By removing the salt shaker, you are taking an important step toward maintaining a low sodium diet.
- Do not add salt to your food during cooking.
- Check the foods you eat for salt content.
- Eat more fresh fruits and vegetables.
- Eat low-salt snacks, such as unsalted popcorn.
![]() Sodium
is found in most processed foods, including canned vegetables and
frozen dinners. Other foods and condiments high in sodium are:
Sodium
is found in most processed foods, including canned vegetables and
frozen dinners. Other foods and condiments high in sodium are:
- Cheese
- Ketchup
- Lunch meat
- Pickles
- Barbecue sauce
- Soya sauce
- Salad dressing
Learn to read food labels to determine how much salt different products contain. Ingredients in prepared food are listed in order – if salt is high on the list of ingredients, it means that there is a lot of salt in the product.
Know What Counts
 |
Potassium
HF patients taking diuretics may need to increase the amount of potassium in their diet. Check with your doctor to determine if you need to increase your potassium intake. Potassium is found in:
- Chicken
- Fish
- Meat
- Bananas
- Citrus juice/fruits
- Prune juice
- Dates
- Raisins
- Mushrooms
- Potatoes
- Spinach
- Squash
- Tomatoes
Fluid Intake
You need to limit the amount of fluids you drink because the more blood there is in your body, the harder your heart works. This extra work puts a strain on the heart of people with heart failure.
It is important to be aware of the amount of fluid you drink – particularly if you are taking diuretics. You should not drink too much or too little fluid. Ask your doctor or nurse to discuss with you the right amount and kinds of fluids you should be drinking. Most people with heart failure should drink no more than 6 to 8 cups of fluid per day. Remember, even the water you drink to swallow your medication should be counted. If your mouth is dry from drinking less fluid, try chewing gum. You can also take sips of water or suck on hard candies to moisten your mouth.
The following items should be considered liquids when you are calculating your daily fluid intake:
- Water
- Ice cubes
- Milk
- Coffee
- Tea
- Juice
- Soft drinks
- Bouillon
- Soup
- Wine
- Beer
- Jell-O
- Popsicles
- Ice cream
- Sherbet
- Frozen yogurt
Amount of fluid permitted daily: ____________ounces/____________mLs.
Food Intake
Now that you must start paying attention to what you eat, follow Canada’s Guidelines for Healthy Eating to ensure you get the right amount of vitamins and nutrients to maintain your health.
Weight Log

Exercise - Take Charge of your Health!
![]() Physical activity is beneficial for your heart and your general health. A
regular program of physical activity will enable you to increase your strength gradually and avoid overtaxing your heart.
Physical activity is beneficial for your heart and your general health. A
regular program of physical activity will enable you to increase your strength gradually and avoid overtaxing your heart.
Exercise can:
- Help increase muscle tone and strength
- Improve your ability to function on a daily basis
- Reduce your HF symptoms (such as shortness of breath and fatigue)
Exercise does not have to be strenuous to be valuable. (In fact, strenuous activities should be avoided.) Before you start any exercise program, be sure to:
- Discuss it with your HF clinic physician or nurse, and set realistic goals
- Plan your exercise period when you feel the most energetic, i.e. first thing in the morning, or after an afternoon nap
- Perform activities, such as stretching, while sitting down whenever possible
- Rest frequently between periods of exercise. You may want to perform shorter activities several times per day, depending on your energy level, for example, a 10-minute walk in the morning, followed by a 10-minute stretch in the afternoon, followed by a 10-minute evening walk
Stretching Exercises
Side-to-side looks: Look straight ahead, slowly turn your head to one side, hold for 10 seconds, then return to centre. Repeat 3 times on each side.
Shoulder shrugs: Sitting in a chair, slowly lift your shoulders up to your ears by squeezing your shoulder blades together, pause, then lower. Repeat 5 to 10 times.
Shoulder circles: Extend both arms sideways at shoulder height. Rotate arms 10 times in small forward circles. Repeat circling back.
Walking
Walking is a simple and effective exercise and is an ideal way to improve your activity level and get more physically fit. Here are guidelines for starting a walking program, but make sure your discuss your plans during a clinic visit before you begin.
| Week 1-2 | Walk 5 to 10 minutes |
| Week 3-4 | Walk 10 to 15 minutes |
| Week 5-6 | Walk 15 to 20 minutes |
| Week 7-8 | Walk 20 to 30 minutes |
Set Personal Goals
- Make exercise part of your daily routine, like brushing your teeth and showering
- Choose a friend to exercise with
- Choose a type of exercise you enjoy
- Keep a journal of your activities. This not only reinforces your exercise habits, it will also show your doctor the progress you are making.
Exercises to Avoid
- Heavy lifting
- Pushing heavy objects
- Shoveling snow
- Climbing stairs
- Sit-ups or push-ups
- Competitive sports
- Heavy housework – washing windows, scrubbing floors
- Racquetball, squash, tennis
STOP Exercising Immediately if you:
- Become short of breath
- Feel weak, tired, or dizzy
- Feel any physical discomfort at all
- Feel your heart rate speeding up
- Have palpitations
- Are in pain
Sexual Activity
Your HF diagnosis does not mean you cannot have sex. In general, you may continue your normal sexual activities. But it is recommended that you avoid having sex:
- If you are tired or tense
- After a heavy meal
- After completing an activity that has already required you to use up a great deal of energy
Daily Exercise Chart
![]()
Download and print our daily exercise chart.
Medications - Your Heart Medication
![]() The
medication your doctor has prescribed is designed to control your
symptoms and improve the efficiency of your heart. Here are some tips
to help ensure you stick to your schedule:
The
medication your doctor has prescribed is designed to control your
symptoms and improve the efficiency of your heart. Here are some tips
to help ensure you stick to your schedule:
- Always take your medication, even if you feel well.
- Take your medications at the same times every day – make it part of your daily routine.
- Never change or stop taking your drugs before asking your doctor about it.
- Your doctor may modify the dose of your medications slightly, depending on what is best for you.
- Have all your prescriptions filled at the same pharmacy – that way, your pharmacist will get to know you and your medical history, and can counsel you appropriately.
| Medication | Action | Side effects | Recommendations |
|
Angiotensin converting enzyme (ACE) inhibitors
Also called: |
• Widens (dilate) blood vessels. |
• Weakness. |
• Take this medication at the same time
each day. |
|
Angiotensin II receptor antagonists*
Also called: |
• Widens (dilate) blood vessels. |
• Weakness. |
• Take this medication at the same time
each day. |
|
Beta-blockers
Also called: |
• Slows heart rate. |
• Weakness, tiredness. |
• Take this medication at the same time
every day. |
|
Diuretics
Also called: |
• Eliminates water and salt (sodium) from
your body. |
• Frequent urination. |
• Take this medication with meals to avoid
stomach upset. |
|
Digitalis/digoxin
Also called: |
• Increases the strength and efficiency of
your heart’s pumping action. |
• Nausea. |
• Take this medication on an empty stomach. • Never change brands or take extra pills. |
|
Nitrates/nitroglycerin & vasodilators*
Also called: |
• Expands your blood vessels, making your heart pump more easily. |
• Fluid retention. |
• Take this medication with liquid at mealtimes. |
|
Anticoagulants & antiplatelets*
Also called: |
• Thins your blood to prevent clots from forming. |
• Hemorrhaging (bleeding), which may result in feelings such as headache, chest, abdomen or joint pain, dizziness, shortness of breath, difficulty breathing or swallowing, swelling, or weakness. |
• Take your dose as soon as possible on the same day if you’ve forgotten, but don’t take a double dose the next day to make up for missed doses. |
|
Inotropic agents
Also called:* |
• Helps your heart pump more effectively. |
• Nausea, vomiting. |
• Inotropic agents are administered intravenously while you are in hospital. |
|
Calcium channel blockers*†
Also called: |
• Used to treat the high blood pressure often associated with heart failure. |
• headaches, facial flushing and dizziness, ankle swelling. |
• These medications are not used often to
treat heart failure. |
|
Potassium*† |
• Since most diuretics remove potassium from the body, heart failure patients who use them are at risk of losing too much potassium. Some patients need to take potassium supplements or pills to compensate for the amount they're losing. |
• ACE inhibitors can actually cause the body to retain potassium, so this needs to be taken into account as well. Patients should check with their doctors to determine their potassium needs. |
• Instead of potassium, sometimes all is
needed to do is eat foods high in potassium, such as bananas. |
*Draft changes pending adoption by CHFN
†Adopted from
Medications Commonly Used to Treat Heart Failure, American Heart
Association
Medical/Medication History
![]() Please use this sheet to record important changes in your medical condition
that you should report during your HF clinic visits. This information
will help your doctors and nurses to better manage your care.
Please use this sheet to record important changes in your medical condition
that you should report during your HF clinic visits. This information
will help your doctors and nurses to better manage your care.
Follow-up Care
![]() If your heart failure has been determined to be stable, you should be
visiting the heart failure clinic every three to six months, or you
may be asked to see your family doctor. Your doctor or nurse will tell
you how often you should visit the clinic. During these visits certain
procedures will be done, including:
If your heart failure has been determined to be stable, you should be
visiting the heart failure clinic every three to six months, or you
may be asked to see your family doctor. Your doctor or nurse will tell
you how often you should visit the clinic. During these visits certain
procedures will be done, including:
- Doing blood tests
- Checking your medications
- Reviewing your diet
- Discussing your exercise routines
If your heart failure has been determined to be unstable, you should be visiting the heart failure clinic daily or weekly. Your doctor or nurse will tell you how often is appropriate. During these visits certain procedures will be done, including:
- Assessing your physical state
- Discussing how well you’re following your medication schedule
- Adjusting your medications, if necessary
- Doing lab tests, if required
- Reviewing your diet
- Discussing what exercise/activity you can do
The clinic’s main aim in seeing you frequently during this time is to ensure you don’t have to be admitted to hospital, and to help you function better at home.
Your clinic's 'telemanagement' program
Telemanagement means that should you need to call your clinic with any questions or concerns, feel free to do so at any time. A clinic nurse will be available to assist you.
Your clinic’s telephone support hotline number is: ____________________
Should you need to call after hours, the pager number is: ________________
Your clinic support group
Your HF clinic has started a support group to help you meet other patients and to learn more about your disease from health care experts.
The next support group meeting will be held: _______________________
The speaker will be: ______________________________________
She/he will be speaking about: ________________________________
We look forward to seeing you there!
Tips for Coping
![]() Controlling the anxiety you may be feeling after being diagnosed with CHF is very
important to your overall well-being. There are many ways to control
anxiety. Here are some suggestions:
Controlling the anxiety you may be feeling after being diagnosed with CHF is very
important to your overall well-being. There are many ways to control
anxiety. Here are some suggestions:
- Write a list of your worries or causes of anxiety. Sometimes just putting pen to paper will help ease your concerns and put things in perspective.
- Try to think of solutions in keeping with the requirements and
restrictions of your illness. For example:
- Surround yourself with positive people
- Learn relaxation techniques – such as deep breathing or meditation
- Talk about your frustrations with those you love and trust
- Consult a resource person – your clinic nurse, social worker or counsellor
- Know and accept your limitations: learn to say no without feeling guilty
- Indulge yourself without feeling guilty. Fulfil a desire in keeping with your lifestyle and pocketbook – for example, go to the theatre, take a holiday, buy an item of clothing or object you’ve been craving
Resources – Booklets
![]() Managing Congestive Heart Failure* (free)
Managing Congestive Heart Failure* (free)
Published by: The Heart and Stroke Foundation of Canada
Heart and Stroke Foundation of Canada
Ontario Chapter
477 Mount Pleasant Road, 4th Floor
Toronto, Ontario M4S 2L9
Living with congestive heart failure: (free)
a guide for people taking Coreg™*
Edited by Peter Liu, MD and Shanas Mohamed, RN
Published by: SmithKline Beecham Pharma
Phone: 1 800 567-1550
SmithKline Beecham Pharma
Medical Information Department
2030 Bristol Circle Place
Oakville, Ontario L6H 5V2
A stronger pump: A guide for people with heart failure (cost:
U.S. $6.50 per copy)
Published by: Pritchett & Hull Associates
Phone: 1 800 241-4925
Pritchett & Hull Associates
3440 Oakcliffe Road, Suite 110
Atlanta, Georgia 30340-3079
Dietary fats and your heart: action plan for a healthy heart*
(free)
Published by: The Becel Heart Health Information Bureau
Phone: 1 800 563-5574
Becel Heart Information Bureau
160 Bloor Street, Suite 1500
Toronto, Ontario M4W 3R2
An owner’s manual for patients with congestive heart failure
(cost: $2.00 per copy)
Contact: Rosa Gutierrez, RN MScN
Walter McKenzie Centre
2C2 Cardiology
8440 – 112 Street
Edmonton, Alberta T6G 2B7
Phone: 403 492-8157
Fax: 403 492-6452
* available in English and French
